Personalized CT-Derived Modeling Guides Choices in Bicuspid Aortic Valve Disease
The computer simulations can help predict who will develop regurgitation or conduction disturbances, new data show..
SAN FRANCISCO, CA—Use of a dedicated patient-specific computer model, derived from CT imaging, to evaluate patients with bicuspid aortic stenosis can identify those best suited for TAVR and those who may be better candidates for surgery, according to the results of a small study.
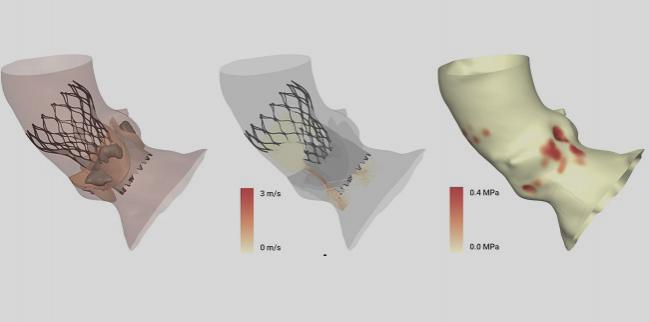
With the technology (HEARTguide, FEops), which uses preoperative CT images to model the aortic root and simulate device performance upon implantation, investigators identified patients who would be at risk for paravalvular regurgitation and conduction disturbance if treated with TAVR.
“The problem is that bicuspid aortic valve is a very heterogenous condition,” lead investigator Cameron Dowling, MBBS (Cardiology Clinical Academic Group/St. George’s, University of London, England), told TCTMD. “Each patient has a different leaflet configuration, raphe location, and calcium distribution. That’s why a one-stop shop is probably not the solution here and why we have been looking at patient-specific computer simulations.”
One of the challenges of TAVR in patients with bicuspid valves is accurately sizing the transcatheter heart valve to the patient’s anatomy, said Dowling.
With this in mind, the researchers used preprocedural CT imaging to develop a model of the aortic root in nine patients with bicuspid aortic valves. Dowling said they then performed finite element analysis, which simulates the interaction between the transcatheter heart valve and the native patient anatomy. “From these simulations, we can see how the transcatheter heart valve is predicted to deform within the native anatomy,” said Dowling. “We then perform computational fluid dynamics to simulate paravalvular regurgitation. Finally, we extract the force that the transcatheter heart valve applies to the native anatomy in order to simulate conduction disturbance.”
Initial Experiences in Small Number of Patients
Today, the researchers presented their initial experiences with the technology during the Medtech and Emerging Technological Trends session at TCT 2019. For the nine patients, the mean age was 79.1 years and the mean STS score was 4.7%. Six of the patients required urgent inpatient treatment, while two had emergent balloon aortic valvuloplasty. Three of the patients had LVEF less than 20%.
In the computer simulation, favorable clinical outcomes were predicted in six patients, but three patients were predicted to have significant paravalvular regurgitation after TAVR. Following discussion in the heart team meeting, the three patients in whom an unfavorable clinical outcome was anticipated with TAVR were instead considered for surgery, which was performed in two of these patients; the third patient was deemed to be at too high risk for surgery and was successfully treated with a Sapien 3 (Edwards Lifesciences) transcatheter heart valve.
For the six patients in whom the computer simulations predicted a favorable outcome, the researchers then performed additional analyses in order to identify an optimal transcatheter heart valve size and implant depth to minimize paravalvular regurgitation and conduction disturbance. In one, a deep implant was necessary to minimize paravalvular regurgitation, so the team inserted a prophylactic permanent pacemaker.
None of the TAVR-treated patients developed moderate paravalvular regurgitation, and none required postprocedure permanent pacemakers. The patient in whom a prophylactic permanent pacemaker was inserted became dependent on the device with underlying third-degree atrioventricular block. To TCTMD, Dowling said they were pleased with how well the simulation and modeling performed, noting that it confirmed their clinical suspicions.
“For this very important patient subset, it’s offering a personalized form of medicine,” senior investigator Stephen Brecker, MD (Cardiology Clinical Academic Group/St. George’s, University of London), told TCTMD. “It’s not just taking something off the shelf.” He also noted that bicuspid aortic stenosis is a heterogenous phenotype and that clinical outcomes with TAVR in heavily calcified bicuspid valves can be “unpredictable.”
Given PARTNER 3 and the Evolut Low-Risk Trial, the two pivotal trials that led to the expanded US indication for low-risk patients, younger patients are now being treated with TAVR and these individuals typically have a higher prevalence of bicuspid valves. Patients with bicuspid aortic valves were excluded from these trials, and treatment with TAVR in this population can only proceed if clinical outcomes are matched by those achieved with surgery, said Brecker.
The researchers had previously validated the technology in 37 patients with pre- and postprocedure CT imaging. In that analysis, the computer simulations were reliable for predicting the transcatheter heart valve frame deformation, the development of paravalvular regurgitation, and the development of conduction abnormalities.
At present, the technology has CE Mark approval in Europe but is not available in the United States. The researchers say that further prospective evaluations are needed, as are software improvements that will allow them to simulate models of all commercially available transcatheter heart valves.
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Dowling C. First in human experience with patient specific computer simulation of TAVR in bicuspid aortic valve morphology. Presented at: TCT 2019. September 25, 2019. San Francisco, CA.
Disclosures
- Dowling reports grant/research support from Medtronic.


Comments