Plaque Protrusion an Infrequent but Troubling Complication of Carotid Artery Stenting
Plaque protrusions were strongly correlated with stroke and point to the need for closed-cell or micromesh stents, study authors say.
Protrusion of plaque into the stent lumen during carotid artery stenting (CAS), though an infrequent complication, illustrates the need for careful periprocedural management and follow-up as well as for ongoing improvements in stent design, a study concludes.
“If plaque protrusion occurs, stent-in-stent placement may [be needed] until the plaque protrusion disappears,” lead investigator Masashi Kotsugi, MD (Ishinnkai Yao General Hospital, Osaka, Japan), commented to TCTMD via email.
In six of nine cases in which plaque protrusion occurred, patients suffered ischemic strokes (one major, five minor), and in eight of nine cases new ipsilateral ischemic lesions were observed on imaging.
Although two previous, smaller studies have shown no correlation between plaque protrusion during CAS and ischemic complications, the researchers conclude that the protrusions are strongly associated with stroke risk despite the use of embolic protection, which was done in all cases. The results raise concerns about the limited efficacy of embolic protection devices in the presence of plaque protrusions and the need for newer stents with smaller open areas, they say.
Minimizing Protrusions Crucial
In their study published April 17, 2017, in JACC: Cardiovascular Interventions, Kotsugi and colleagues sought to clarify the frequency and prognosis of plaque protrusions in CAS by analyzing data from 328 patients who were treated under IVUS guidance at their hospital or an affiliated center between October 2007 and March 2016. Multiple types of stents and embolic protection devices were used.
At 30 days, the rate of ipsilateral ischemic stroke was 2.8% and the rate of transient ischemic attack was 2.6%. No patients died, and in most cases of stroke, the symptoms were observed immediately after dilatation. New ischemic lesions were noted in 35.7% of patients on diffusion-weighted imaging (DWI) within 48 hours of the procedure. Surprisingly, a comparison of plaques known to be stable versus those known to be unstable revealed no difference in the incidence of new ischemic lesions (P = 0.49).
Analysis by stent type, however, did indicate a difference in the rate of ipsilateral ischemic lesions on DWI, with more of these type of lesions observed when open-cell stents were used in comparison to closed-cell stents (39.1% vs 26.7%; P = 0.016).
According to Kotsugi and colleagues, the results suggest that minimizing plaque protrusion “is necessary to prevent periprocedural ischemic stroke.” They also hypothesize that placement of open-cell stents with a high radial force may disintegrate soft, unstable plaque, thus causing the protrusions.
The study authors say their strategy for managing plaque protrusion is to perform IVUS to check for large-volume protrusions. If the protrusions are “convex,” they perform stent-in-stent placement using closed-cell stents until the protrusion disappears. If the protruding plaque is “nonconvex,” they recommend observation for 5 to 10 minutes. At that point, if there is no change, careful clinical follow-up is considered within 30 days after CAS, they note. If the nonconvex plaque does enlarge, however, stent-in-stent placement is recommended until the protrusion disappears.
Caveats and Closed Cells
In an editorial accompanying the study, William A. Gray, MD (Lankenau Heart Institute, Wynnewood, PA), cautions that the retrospective study has important limitations. One is that the investigators found 27 cases of plaque protrusion on IVUS, but only nine cases on angiography. Their study protocol required confirmation by both modalities, however, “which cut by two-thirds the incidence of IVUS [plaque protrusion] and which will clearly affect many of the subsequent associations and conclusions.”
Gray also notes that the study was not core-lab controlled, MRI was not routinely used before and after procedures, and the assessors were not blinded. Additionally, the study authors did not mandate use of specific stents and did not perform routine independent neurological assessment of the clinical outcomes. Importantly, he adds, by treating plaque protrusion with stent-in-stent placement in approximately half of the cases, they potentially changed the clinical and imaging outcomes.
According to Gray, the association between stent type and plaque protrusion “is likely,” but may not be as strong as the authors contend.
Gray agrees, though, that that when the study is paired with emerging data showing reductions in both plaque protrusion and new ischemic lesions with mesh-covered stents, “the case begins to grow for such improvements in stent design.”
In the United States, the SCAFFOLD trial is evaluating a mesh-covered open-cell stent in patients at high surgical risk, and two other similar trials using different mesh technologies are imminent, Gray notes.
Kotsugi and colleagues add that on the basis of their study, they have changed their protocol and now use a closed-cell stent first when the plaque is evaluated and found to be unstable prior to the procedure.
To TCTMD, Kotsugi said “CAS should be performed using a stent with as small a free cell area as possible to prevent plaque protrusion,” adding that micromesh stents are expected to contribute greatly to the prevention of plaque protrusion and may become the new standard stent for CAS.
Proving an Old Hypothesis
The observation of carotid plaque protrusion goes back over 20 years, said noted vascular surgeon Frank J. Veith, MD (Cleveland Clinic, OH, and New York University, NY), and it was the impetus for widespread interest in embolic protection devices. In a paper published in the mid-1990s, Veith and colleagues hypothesized that as flow was restored and protection devices were removed, protrusions could continue to break off and might be responsible for some delayed strokes.
To TCTMD, Veith said ongoing studies of mesh-covered stents are promising and, combined with reversal of flow and proper patient selection, suggest “a bright future” for carotid stenting with potential to reduce the stroke rate significantly.
“It’s pretty clear that there are more strokes with carotid stenting than there are with endarterectomy, particularly in the high-grade symptomatic patients. This article sort of proves . . . our hypothesis from the beginning,” he said. “Presumably, many of these late strokes will be prevented with the mesh-covered stents currently being studied. I don’t think they will prevent all of the strokes, but they will make carotid stenting safer.”
But Veith said only time will tell how things shake out over long-term follow-up with the newer stents.
“It’s a work in progress,” he said. “These stents have different-sized pores, different flexibility, different properties in general, so which is going to be the best? I don’t know.”
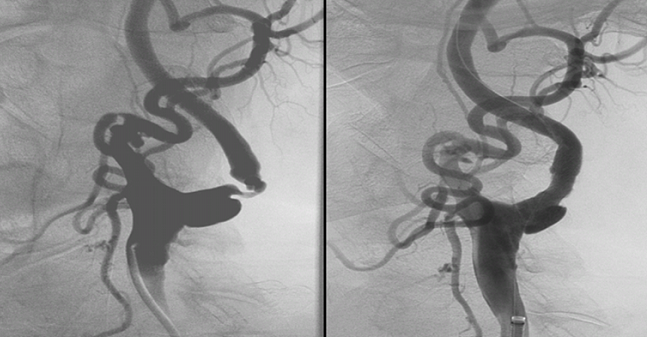
Photo Credit: Gray WA. Extracted from: Are mesh covered stents the future of CAS? Evaluation with OCT and IVUS. TCT 2016.
L.A. McKeown is a Senior Medical Journalist for TCTMD, the Section Editor of CV Team Forum, and Senior Medical…
Read Full BioSources
Kotsugi M, Takayama K, Myouchin K, et al. Carotid artery stenting: investigation of plaque protrusion incidence and prognosis. J Am Coll Cardiol Intv. 2017; 10:824-831.
Gray WA. Blurred lines: assessing the stent as provocateur in carotid intervention. J Am Coll Cardiol Intv. 2017; 10:832-833.
Disclosures
- Kotsugi and Veith report no relevant conflicts of interest.
- Gray reports consulting for Boston Scientific, Contego, Medtronic, Silk Road Medical, and WL Gore.


Comments