Platelet Reactivity High in Most Patients Who Develop Stent Thrombosis
Neither maintenance therapy with antiplatelet agents nor preloading before PCI to treat stent thrombosis had an effect on platelet reactivity.
High platelet reactivity is widespread among patients presenting with stent thrombosis, according to results from a European registry. The findings add to several prior observations that platelet reactivity is frequently elevated in patients after treatment for stent thrombosis as well.
The study authors, led by Thea C. Godschalk, MSc (St. Antonius Hospital, Nieuwegein, the Netherlands), found that three out of four patients (76%) presenting with STEMI due to definite stent thrombosis had high platelet reactivity as measured by P2Y12-inhibitor assay. Additionally, 13% had high platelet reactivity on aspirin.
“This raises concerns that the majority of patients with [stent thrombosis] have suboptimal platelet inhibition undergoing immediate PCI,” they write.
The findings will come as no surprise to researchers who have long championed the importance of recognizing high platelet reactivity and devising strategies to improve P2Y12-receptor inhibition, noted Paul Gurbel, MD (Inova Heart and Vascular Institute, Falls Church, VA). Gurbel’s team first identified high platelet reactivity and incomplete P2Y12-receptor inhibition as risk factors for subacute stent thrombosis in a 2005 paper published in the Journal of the American College of Cardiology.
“To me this is basically rediscovering the wheel; it’s no epiphany to me that platelet reactivity would be high when patients come in with a stent thrombosis,” Gurbel said in an interview with TCTMD. “We have already shown that it’s high after stent thrombosis.”
Importantly, Gurbel said nothing much has changed in the last 10 or 12 years since the importance of platelet reactivity first came to the attention of researchers.
“We’re still not measuring [it] in patients as a standard of care,” he observed. “We’re not moving the needle.”
Aspirin Loading, Stronger Antiplatelet Agents May Help
For the new study, researchers evaluated platelet reactivity in 129 stent thrombosis patients presenting with STEMI who were undergoing immediate PCI. The patients were part of the PRESTIGE registry, which enrolled from nine European Union countries. Platelet reactivity was measured with the VerifyNow P2Y12 or VerifyNow Aspirin (Accriva Diagnostics, San Diego, CA) assays or the Multiplate adenosine diphosphate (ADP) assay (Roche Diagnostics).
Not only was high platelet reactivity on P2Y12 inhibitors identified in most patients presenting with stent thrombosis, it also was found to be similar regardless of whether patients were on maintenance therapy with a P2Y12 inhibitor at presentation or not, and no matter whether patients were loaded with a P2Y12 inhibitor prior to PCI or not. Likewise, high platelet reactivity was similar on aspirin assay regardless of whether patients were on maintenance aspirin at presentation or not. However, unlike P2Y12 inhibitors, loading with aspirin prior to PCI appeared to show some benefit, with patients who were loaded having lower platelet reactivity than those who were not (P = 0.006). At 1 to 3 days after PCI, the percentage of patients who still had high platelet reactivity was dramatically decreased in all groups.
According to Godschalk and colleagues, the findings suggest that the platelet activation caused by stent thrombosis is so great that it essentially overrides the antiplatelet effects of P2Y12 inhibitors, specifically clopidogrel, which was used in the majority of patients.
“Possible mechanisms may be an increased level of immature platelets or increased platelet turnover immediately before ST occurs, as has previously been suggested for patients presenting with spontaneous STEMI where an increased level of reticulated platelets and higher platelet turnover were associated with an insufficient response to [aspirin therapy],” they write.
Additionally, they say their finding that aspirin loading appeared to lower platelet reactivity while P2Y12 loading did not may be related to onset-of-action times, which are faster for aspirin. Another option to consider, they add, is direct-acting, strong, intravenous P2Y12 inhibitors such as cangrelor (Kengreal; Chiesi USA) or glycoprotein IIb or IIIa receptor antagonists.
A Matter of Timing
In an accompanying editorial, Anna Maria Gori, PhD (University of Florence, Italy), and colleagues advocate for more comprehensive platelet function tests rather than individual P2Y12 or aspirin assays, with the idea that a test measuring global platelet reactivity could detect more patients at risk. “Another emerging question,” they write, “is whether a single time point of platelet function assessment is accurate to define patients ‘resistant’ to antiplatelet treatment.”
In fact, in a paper published earlier this month in the Journal of Interventional Cardiology, researchers go so far as to say it is “far-fetched” to depend on a single measurement of platelet function to reliably predict the risk of stent thrombosis given its multifactorial etiology.
In their study of 357 ACS patients who suffered cardiogenic shock or cardiac arrest, platelet function testing after PCI was moderately able to identify those at risk for early stent thrombosis. They suggest that it may best be used in this population as a means of risk-stratifying patients, but not as a routine screening procedure.
Gurbel said the issue is complicated and goes back to why the needle hasn’t moved.
“The reason we haven’t moved the needle is because we haven’t shown that measuring platelet reactivity changes the outcome if you alter therapy based on it,” he observed.
The two largest studies that have attempted to look at this issue, GRAVITAS and ARCTIC, were both negative and underpowered, raising doubts about tailoring antiplatelet therapy based on platelet function testing results.
“The totality of the evidence is pretty conclusive that platelet reactivity is a risk factor for thrombotic events,” Gurbel said, noting that while high platelet reactivity appears to be modifiable, the mechanisms for modifying it remain unclear and at the mercy of positive, randomized trials.
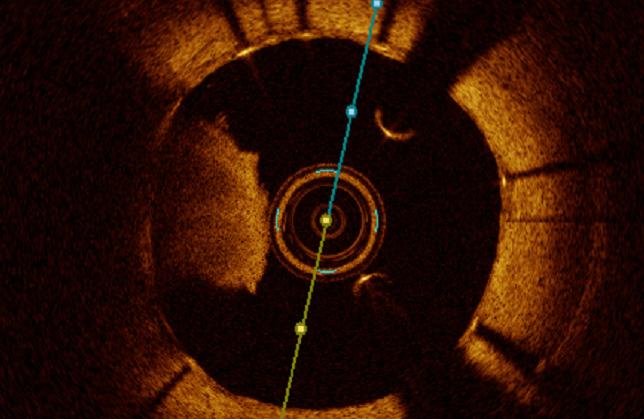
Photo Credit: Mitsuaki Matsumura. Intravascular Imaging Core Lab, Cardiovascular Research Foundation.
L.A. McKeown is a Senior Medical Journalist for TCTMD, the Section Editor of CV Team Forum, and Senior Medical…
Read Full BioSources
Godschalk TC, Byrne RA, Adriaenssens T, et al. Observational study of platelet reactivity in patients presenting with ST-segment elevation myocardial infarction due to coronary stent thrombosis undergoing primary percutaneous coronary intervention: results from the European PREvention of Stent Thrombosis by an Interdisciplinary Global European Effort Registry. J Am Coll Cardiol Intv. 2017;10:2548-2556.
Gori AM, Giusti B, Marcucci R. An unresolved question antiplatelet treatment driven by platelet function in ST-segment elevation myocardial infarction patients. J Am Coll Cardiol Intv. 2017;10:2557-2559.
Tilemann L, Mohr SK, Preusch M, et al. Platelet function monitoring for stent thrombosis in critically III patients with an acute coronary syndrome. J Interven Cardiol. 2017;Epub ahead of print.
Disclosures
- Godschalk, Gori, and Tileman report no relevant conflicts of interest.


Comments