POP-HT: Physician-Guided Self-Monitoring Improves BP After Hypertensive Pregnancy
The trial should signal a paradigm shift in how women with hypertensive disorders of pregnancy are managed long-term.
PHILADELPHIA, PA—Equipping new mothers with the tools to self-monitor their blood pressure, as well as smart tech for checking in with a doctor remotely for medication changes, leads to better BP control after a hypertensive pregnancy, according to the British POP-HT trial. The intervention also reduced hospitalizations for hypertension during the busy first months postpartum, investigators say.
Moreover, cardiac imaging at the 6-month mark suggested that women in the intervention arm had more signs of reverse cardiac remodeling, which suggests that this kind of guided self-monitoring might translate into better long-term CV outcomes for an underserved area in cardiovascular disease prevention.
“Basically the women who had the intervention had reduced ventricular mass, they had improved systolic function, had improved diastolic function, and they had changes also in left atrial size,” said Paul Leeson, PhD (University of Oxford, England), in a press conference prior to the presentation here at the American Heart Association (AHA) 2023 Scientific Sessions. “This is consistent with beneficial remodeling associated with improved outcomes over time.”
The study was simultaneously published in JAMA.
Discussant Anastasia Mihailidou, PhD (Royal North Shore Hospital, Sydney, Australia), noted that women in the intervention arm were much more adherent than most patients on antihypertensives, with the bonus that the telemonitoring appears to make it easy to keep communication lines open between patients and their physicians without requiring travel for an office visit and interruption of childcare.
Mihailidou said another factor in favor of this type of intervention is that women tend to have a higher rate of white-coat hypertension than do men, making ambulatory out-of-office measurements of particular importance.
The study is a timely reminder, Mihailidou said, “that physicians and patients are not aware that hypertension disorders of pregnancy are a critical and important long-term risk for these women [and that] they need to be monitored lifelong.”
POP-HT Remote Monitoring Results
Leeson and colleagues led by Jamie Kitt, MBBCh (University of Oxford), randomized 220 women (mean age 32.6 years; 8% Asian) who were on an antihypertensive medication following delivery with a diagnosis of preeclampsia (60%) or gestational hypertension (40%) during pregnancy. The median duration of antenatal hypertension medication treatment was 4 to 5 months, with 70% of women having discontinued medication at 6 months.
They were enrolled around the time of delivery and randomized to physician-optimized self-management or to usual care. BP readings in the intervention group were taken using a Bluetooth-enabled device provided to study participants and were uploaded to a smartphone app that transmitted the BP data a secure web-based platform, with notifications to downtitrate, continue current dosing, or seek out clinician advice on uptitration.
“There was a predefined algorithm to guide titration of medication, which was based on the [UK guidelines],” Leeson told TCTMD. “That digital optimization was to enable a conversation between the mother and the physician to guide how you change the medication dose.”
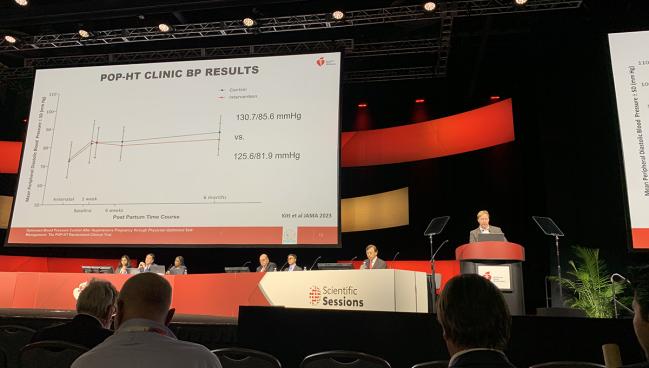
The mean adjusted 24-hour BP at 9 months postpartum was 114 mm Hg systolic/71.2 mm Hg diastolic in the intervention group and 120.3 mm Hg systolic/76.6 mm Hg diastolic in the control group (P < 0.001). Similarly, the mean adjusted 24-hour systolic BP was 6.51 mm Hg lower in the intervention group compared with controls (P < 0.001).
Mean clinic diastolic BP levels at 1 week, 6 weeks, and 6 to 9 months also were lower in the intervention group. By week 6, systolic blood pressure was also lower compared with controls.
Of 41 total hospital readmissions in the 14 days after discharge, fewer of them occurred in the intervention group than in the control group (7% vs 27%; P < 0.001). The number need to treat to avoid one postnatal hospitalization for hypertension was 5.
On cardiac imaging, the intervention group showed statistically significant improvements in left ventricular mass, left ventricular ejection fraction, left ventricular global longitudinal strain, left atrial volume, left ventricular relative wall thickness, and average E/E ratio, as compared with the control patients.
This is the first randomized trial evidence to show that blood pressure interventions in the first few weeks can have medium- to long-term benefit. Jamie Kitt
Kitt, who presented the findings in the late-breaking science session, said the accumulating evidence suggests that the postpartum period appears to be a critical window to reduce long-term risk.
“This is the first randomized trial evidence to show that blood pressure interventions in the first few weeks can have medium- to long-term benefit,” he added. If the benefits seen in diastolic and systolic BP were maintained long-term, coupled with the imaging evidence of improvement, Kitt said it would be expected that women could see a 20% reduction in lifetime CV risk with this type of intervention.
Generalizability and Other Questions
“Before you can have implementation, you really want to know it's robust,” Mihailidou told TCTMD when asked about widespread applicability of the POP-HT protocol.
She noted that the all-British cohort was not culturally diverse enough and said the cohort is too small overall to draw firm conclusions as to whether the high rates of adherence can be replicated elsewhere.
“Also, they've got a really great system in terms of monitoring and following up that has to be replicated elsewhere with other health systems and that's where it may fall apart unless you've got the backup. Having said that, it's a great opportunity to bring in the bigger multidisciplinary team . . . pharmacists, nurses, and allied health people,” Mihailidou added.
In his presentation, Kitt said the study “identifies a potential need for a paradigm shift in the way women with hypertension in pregnancy are managed in the postnatal period.”
In response to a question following his presentation, Kitt noted that there were very high rates of breastfeeding in both arms of the study, with about 70% continuing to breastfeed at 6 months, suggesting no significant negative impact of antihypertensive therapies.
L.A. McKeown is a Senior Medical Journalist for TCTMD, the Section Editor of CV Team Forum, and Senior Medical…
Read Full BioSources
Kitt J, Fox R, Frost A, et al. Long-term blood pressure control after hypertensive pregnancy following physician-optimized self-management: the POP-HT randomized clinical trial. JAMA. 2023;Epub ahead of print.
Disclosures
- The study was funded by the British Heart Foundation.
- Leeson reports no relevant conflicts of interest.





Comments