Preliminary Results Suggest Benefit of Splanchnic Nerve Ablation in HFpEF
A more-definitive look awaits in the sham-controlled portion of REBALANCE-HF, but this is promising, Biykem Bozkurt says.
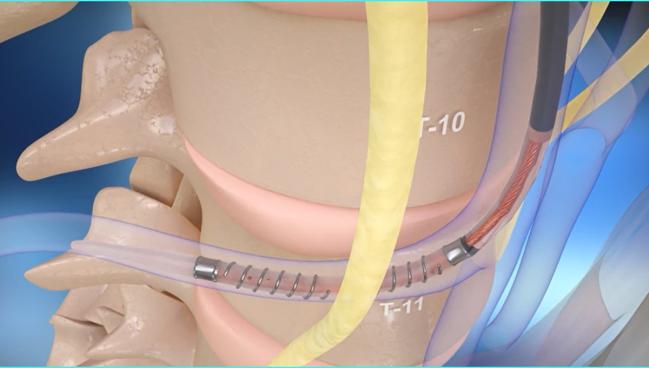
Photo Credit: Adapted from Fudim M. Mechanistic overview of SAVM: splanchnic ablation for volume management in heart failure patients. Presented at: THT 2023. Boston, MA.
BOSTON, MA—Ablation of the greater splanchnic nerve shows promise as a treatment for patients who have heart failure with preserved ejection fraction (HFpEF), according to results observed in the roll-in cohort of the REBALANCE-HF trial.
One month after the procedure, pulmonary capillary wedge pressure (PCWP) was lower during a leg raise and exercise. There were also improvements seen in health status, functional capacity, and symptom burden through 6 months.
Marat Fudim, MD (Duke University, Durham, NC), who presented the results here at the Technology and Heart Failure Therapeutics (THT) 2023 meeting, noted that the study is limited by the lack of a control group and the lack of blinding, adding that “the findings presented here require confirmation in the ongoing randomized, sham-controlled portion of the REBALANCE-HF study.”
What has been observed so far, however, is encouraging, commented Biykem Bozkurt, MD, PhD (Baylor College of Medicine, Houston TX). Bozkurt is editor-in-chief of JACC: Heart Failure, in which some of the findings will be published.
Splanchnic nerve denervation is a novel intervention for volume redistribution in patients with HFpEF, she told TCTMD, and it was previously shown that it may be effective in those with increased filling pressures at rest. These new data, she said, demonstrate that it also could be effective in those with increases in filling pressures induced by leg elevation or exercise.
There are remaining areas of uncertainty, such as how the volume redistribution is occurring and which patients will be the best candidates for ablation, but “it’s promising,” Bozkurt said.
Preventing Blood Redistribution During Exercise
The splanchnic compartment, containing the liver, spleen, stomach, and intestines, serves as the body’s main blood reservoir, with 30% to 40% of the total intravascular blood volume found there. The area is “highly innervated” with autonomic nerve fibers, including the splanchnic nerves, Fudim said.
During exercise, activation of the sympathetic nervous system leads to a shifting of blood from the splanchnic bed into the central circulation, which increases intra-cardiac pressures and stressed blood volumes. The idea behind splanchnic nerve ablation is that it will block this process and keep blood in the splanchnic reservoir. Fudim said multiple single-center studies have demonstrated its impact on lowering filling pressures in patients with heart failure.
The ongoing REBALANCE-HF trial is the largest feasibility study of the technique in patients with HFpEF, Fudim said. It includes both an open-label, roll-in phase and a randomized, sham-controlled phase. Enrollment for the latter phase has been completed, but the results will not be presented until the end of the year, Fudim said.
He presented the results among the 26 patients (median age 71 years; 73% women) included in the roll-in cohort, enrolled across 18 centers to provide experience with the procedure before the randomized phase. Most patients (88.5%) had NYHA class III symptoms, and most had an LVEF of 50% or more; at the end of the study, the protocol was amended to allow a few patients with LVEF between 40% and 50%. Median LVEF was 59%.
Patients were on stable guideline-directed medical therapy and comorbidities were well-managed. Medical therapy included a loop diuretic in 81%, a beta-blocker and a mineralocorticoid receptor antagonist in 69%, a sodium-glucose cotransporter 2 (SGLT2) inhibitor and ACE inhibitor/ARB in 38%, and an angiotensin receptor-neprilysin inhibitor (ARNI) in 8%.
The ablation procedure was performed via transfemoral access using the Satera system (Axon Therapies), which employs radiofrequency energy.
The primary hemodynamic endpoint was PCWP, and mean values were lower a month after ablation during leg elevation (21.2 vs 23.6 mm Hg), at low-level exercise at 20 watts (30.8 vs 36.6 mm Hg), and at peak exercise (33.1 vs 39.2 mm Hg; P < 0.05 for all).
There were also numerical improvements in exercise duration, the amount of wattage achieved at peak exercise, and workload-normalized PCWP at 1 month, although the differences did not reach statistical significance.
These changes were accompanied by gains in patient-centered outcomes. The proportion of patients in NYHA class I/II was 60% by 1 month (compared with 8% at baseline), and mean Kansas City Cardiomyopathy Questionnaire (KCCQ) overall score rose from 46 to 69 points. More than 70% of patients had at least a 15-point bump in KCCQ score, Fudim said. “Please keep in mind this is a single-arm, open-label study,” which could have influenced the findings, he noted. “But nevertheless the improvements were quite impressive all the way out to 6 months.”
In addition, 6-minute walk test distance gradually increased over the course of follow-up, rising from a mean of 267 meters at baseline to 343 meters at 6 months (P < 0.05).
As for safety of the procedure, there was one serious adverse event related to the device or procedure within 1 month—worsening heart failure. Through up to 12 months, 53.8% of patients reported at least one adverse event, with four serious device-related or vascular events (15.4%). There were no deaths and no cases of acute kidney injury requiring renal replacement therapy.
Fudim said some patients experienced pain in the area of the ablation and orthostatic hypotension, but that all of those events were limited.
Future Work
During a panel discussion, Bozkurt asked Fudim about the mechanism of benefit of splanchnic nerve ablation and whether it’s related to prevention of the autotransfusion of blood into the general circulation or to a change in the relative proportion of stressed and unstressed blood volume.
“The idea is that if we are able to prevent just that 100 ccs of blood transfusion that happens with everybody exercising, when the stress kicks in and we shift the blood into the chest, . . . that’s probably the hemodynamic benefit of this,” Fudim responded.
One solution will not fit all [HFpEF] phenotypes, and I think that’s something that we are increasingly acknowledging as we’re doing more research in this space. Marat Fudim
To TCTMD, Bozkurt said the study showed a good safety profile, though noted that a more-definitive assessment will come in studies with larger sample sizes.
“This is a potentially promising modality,” she said. “The question is going to be identifying the right phenotype of patient who would benefit from this” with the right balance of risks and benefits. She noted that a significant proportion of patients with HFpEF are volume-overloaded, suggesting that patients with repeated hospitalizations due to congestion or those who are refractory to diuretics could be candidates for the procedure.
“This potentially could describe about a quarter to almost half of our HFrEF patients,” Bozkurt said. But, she added, it remains to be determined what impact splanchnic nerve ablation will have on the background of improving guideline-directed medical therapy for HFpEF, including growing use of SGLT2 inhibitors.
Fudim said that his team is planning to do a secondary analysis that will look at responders and hyperresponders to ablation, using predefined changes in NYHA class, KCCQ score, 6-minute walk test distance, body weight, NT-proBNP, and PCWP. “Because we want to then, of course, give that therapy not to everybody or to a very broad cohort, as we did in the initial study, but roll it out to specific phenotypes, as it is done now with other therapies such as interatrial shunting,” he explained.
HFpEF is a heterogeneous syndrome, he stressed during his presentation: “One solution will not fit all phenotypes, and I think that’s something that we are increasingly acknowledging as we’re doing more research in this space.”
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Fudim M. Endovascular ablation of the right greater splanchnic nerve in heart failure with preserved ejection fraction: updated results of the REBALANCE-HF trial roll-in cohort. Presented at: THT 2023. March 21, 2023. Boston, MA.
Disclosures
- REBALANCE-HF is sponsored by Axon Therapies.
- Fudim reports receiving consulting fees/honoraria/speaking fees from Axon Therapies.
- Bozkurt reports serving on a clinical endpoints committee for Abbott Vascular, receiving consulting fees/honoraria/speaking fees from AstraZeneca, Sanofi Aventis, scPharmaceuticals, and Vifor, and serving on a data and safety monitoring board for LivaNova.





Comments