The Prickly Problem of Permanent Pacing After TAVR: One Hospital Pitches a Protocol
Vexed by the prevalence of AV block following TAVR, one EP department has offered a solution. Naysayers, however, say the approach is overly cautious.
Physicians at one US hospital are attempting to address electrical complications that develop after transcatheter aortic valve replacement, focusing on a new protocol to manage atrioventricular (AV) block and pacemaker implantation.
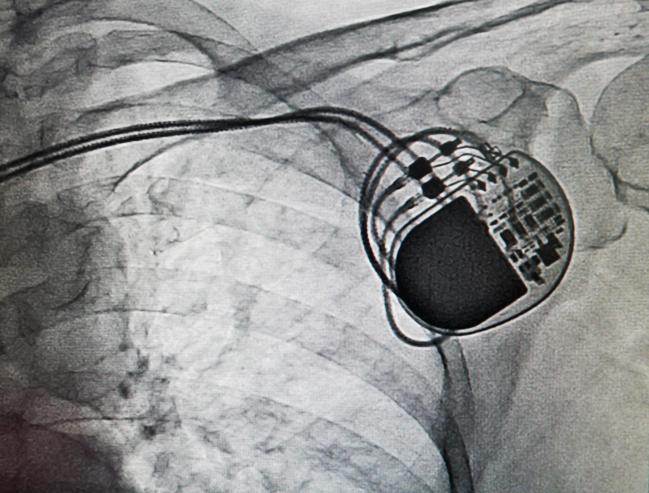
The approach, developed by physicians at The Christ Hospital (Cincinnati, OH), recommends all patients receive 12-lead ECGs immediately before and after TAVR, as well as each morning they are in the hospital. Most importantly, the protocol places a greater emphasis on the use of temporary pacemakers, with electrophysiologists (EPs) recommending that “all patients get effective, reliable, well-secured temporary pacemakers upon leaving the operating room.”
The temporary pacer would stay in place at least until the next day, with the decision to remove it dependent upon a review of telemetry and the 12-lead ECG.
Edward “Jay” Schloss, MD, the electrophysiologist who developed their approach with input from other physicians at the hospital, said the EP community remains “vexed” by AV block after TAVR. The proposed protocol, which is not written in stone, was developed so that they might “get out it out into the community, kick it around, and have it percolate to the point where it might be discussed and revised,” he explained.
“The reason I’m banging the drum is because it surprises me that year after year this issue has been in play and it really hasn’t bubbled up to the point where people are talking about it publicly,” Schloss told TCTMD. “It’s not at meetings, there’s no consensus statement, there’s no prospective trials. There’s been a few articles written about it, but those articles haven’t had a lot of impact.”
Dean Kereiakes, MD, who practices at the same hospital, also lamented the lack of clinical direction and standardization for monitoring and treating patients for conduction disturbances following TAVR. As one of the original clinical centers for the PARTNER 2 trial comparing TAVR using the balloon-expandable Sapien XT valve (Edwards Lifesciences) with aortic valve surgery in intermediate-risk patients, Kereiakes said they frequently placed a temporary balloon-tipped pacing wire via the femoral approach and would pull the pacer at the end of the procedure.
“That’s fine if there are no conduction defects, but it’s really a problem because a number of these patients have baseline first-degree block, bundle branch blocks, and even atrial fibrillation, which in some analyses has shown to be an independent predictor of the need for a new pacemaker,” said Kereiakes. Such patients, he added, represent a significant number of those seen in clinical practice.
I do think there is a need for greater focus and a need for guidelines. No hospital wants to drop another $60,000 for a pacemaker, and nobody wants to put in a device that’s not indicated, particularly in a patient with a long life expectancy. Dean Kereiakes
“I do think there is a need for greater focus and a need for guidelines,” Kereiakes told TCTMD. “No hospital wants to drop another $60,000 for a pacemaker, and nobody wants to put in a device that’s not indicated, particularly in a patient with a long life expectancy.”
The EP Perspective
Speaking with TCTMD, Schloss said patients who develop slow heart rates typically do so over time. With TAVR, where the implanted valve can press against the AV node and disrupt and/or disconnect electrical conduction between the atrium and ventricle, heart block can be a flat-out medical emergency.
“To fix it, if you don’t already have a pacer in place, is a big deal,” said Schloss. “You can’t do it at the bedside, you can’t do it with drugs. You need a specialized team to come in, not unlike an acute MI. You need to mobilize the team, race people in, and get the patient under fluoroscopy. So going about this appropriately is important, because there can be a pretty significant impact if you don’t.”
He added that patients who go home with undiagnosed and untreated heart block can fall, which can lead to broken hips and other major accidents such as head injuries and possibly death. Schloss said their protocol is designed to manage and prevent these emergencies and, at the same time, to minimize the use of unnecessary pacemakers and hospital resources.
“Interventionalists are can-do people,” said Schloss. “And not to generalize too much, but if they thought a pacemaker might be necessary, they’d say, sure, put the pacemaker in. Electrophysiologists have lived in a highly regulatory environment. We have very strong rules about who gets and doesn’t get a medical device. We’re used to being reviewed, and there have been [Department of Justice] actions for people putting in too many devices. So we’re really sensitive. On top of that, if we put a device in, this is something you have to care for the rest of the patient’s life.”
Interventionalists are can-do people. And not to generalize too much, but if they thought a pacemaker might be necessary, they’d say, sure, put the pacemaker in. Jay Schloss
Kereiakes said the lack of clinical guidelines and standardization of monitoring for AV block is what led them to work directly with their electrophysiology colleagues. And while interventionalists at his institution are now typically following EP advice and using temporary pacemakers, they will occasionally opt to override it, Kereiakes said, in certain, low-risk patients. In a patient with no conduction defects, narrow QRS intervals before and after the procedure, and no complications during the procedure, Kereiakes said they remove the temporary pacing wire no later than the next day.
In such low-risk patients, however, Schloss said he is in agreement with Kereiakes. “We’re all for removing the temporary pacers the next morning in the appropriately selected patients,” he told TCTMD.
As part of the proposed protocol, the EPs recommend all patients with a QRS > 120 ms before or after the procedure, as well any patients with transient or persistent AV block, keep the temporary pacer in place at least until day 2. Individuals with new conduction abnormalities, they say, should also recover in the intensive care unit. For those with new left bundle branch block or other advanced AV conduction disturbances not receiving a pacemaker, a 4-day hospital stay with inpatient telemetry is recommended. Finally, permanent pacemaker implantation on the same day as TAVR “should be rare, and only in the highest risk patients.”
Schloss said long-term complications from a pacemaker might not be a major issue for an 85-year-old patient, but noted that TAVR is moving into intermediate-risk patients and maybe low-risk surgical patients. “We’re going to have people with TAVR who are going to live for 20 or 30 years,” he said. “In these patients, an unnecessary pacemaker is a really, really bad idea.”
Judy Mackall, MD (UH Cleveland Medical, OH), an electrophysiologist, said the proposed protocol is a “good idea,” noting it would be helpful to see it prospectively studied and reviewed. “At our hospital, particularly for patients with preexisting right bundle branch block, we’ve been looking at how to move them through the system in the most efficient way,” she said.
To TCTMD, Mackall said patients with preexisting right bundle branch block at UH Medical Center are designated “high risk” for complete heart block. In such patients, an actively secured temporary pacing lead is important, although they will remove the pacing wire after 24 hours as long as they can safely do so. “The idea is to try to avoid same-day permanent pacemaker implants, because same-day implants carry a higher risk for the patient,” she said.
For Mackall, the decision by physicians at The Christ Hospital to remove the temporary pacer based on ECG changes that occur during or after the procedure is reasonable. For the lowest-risk patients—those with unchanged and narrow QRS interval with normal conduction—who receive a Sapien valve, the risk of heart block after the procedure is low, she noted. In such patients, Mackall was cautious but said physicians “could feel comfortable” removing it after the procedure.
Protocol Best for Older TAVR Systems?
Speaking with TCTMD, interventional cardiologist John Webb, MD (St. Paul’s Hospital, Vancouver, Canada), said the incidence of heart block depends on a number of factors, but the most relevant factor is the type of valve used during the procedure. Although the exact rate of pacemaker implantation varies, the original Edwards Sapien valve had the lowest rate. Pacemaker implantation rates with Edwards Lifesciences’ Sapien XT valve are approximately 5% to 10%, although the next-generation Sapien 3 valve has a higher rate than its predecessor, studies have shown.
In contrast, pacemaker implantation rates are markedly higher with Medtronic’s self-expanding CoreValve and Boston Scientific’s Lotus mechanically expanded valve system. The implantation rate with CoreValve ranges from 15% to 30%, said Webb, with some estimates even higher. The company’s next-generation valve, known as Evolut R, is said to improve upon this rate of implantation. The Lotus valve, still investigational in the United States but available in Europe, results in permanent pacemakers in approximately 30% to 40% of those who receive the device.
At St. Paul’s Hospital, Webb told TCTMD the pacemaker rate is less than 6%. Such a low rate is achieved by using “valves less likely to cause heart block” and not positioning the device too low in the left ventricular outflow tract (LVOT). With pacemaker rates as low as these, he doesn’t think the cautious approach proposed by The Christ Hospital team is warranted.
“We wouldn’t dream of keeping patients in hospital for several days,” he said. “They’re suggesting a temporary wire overnight, but I would estimate that 2% of our patients have a temporary wire overnight. It’s rare. And 80% of our transfemoral patients are discharged the following morning.”
Tamim Nazif, MD (Columbia University Medical Center, New York, NY), another interventional cardiologist, also called the protocol “conservative,” noting that it appears best suited for older TAVR systems, particularly the self-expanding CoreValve.
“Because the [pacemaker] rates with CoreValve were so much higher, and because it can continue to expand—[even] after the procedure—some of the heart block and other issues can occur late,” said Nazif. “It’s unpredictable, it happens at a higher rate, and it might happen at a time after the procedure. So the protocol [in Ohio] was standard of care that we followed, and a lot of other people followed, with the first-generation CoreValve device.”
With Sapien, though, patients who will require a permanent pacemaker typically experience AV block early, usually at the time of TAVR, making it more predictable to manage. “So, unless they have actual heart block at the time of the procedure, or a new left bundle branch block with first-degree heart block with bradycardia—those two scenarios—we would pull the temporary pacemaker out right at the time of the procedure,” said Nazif. “We wouldn’t keep it in at all, and certainly not for 24 or 48 hours. It’s really the minority of patients.”
Nazif told TCTMD that even with first-generation devices, few patients left their lab with the temporary pacemaker in place. “That’s important, because right now the whole name of the game has shifted to expedited recovery and discharge,” he said.
Following the protocol outlined by The Christ Hospital would slow patient recovery, particularly since the temporary pacemaker would require venous access through the neck (either via the jugular or subclavian vein) for 2 days, said Nazif. Their expedited recovery process aims to discharge patients the day after TAVR, which is predicated on not leaving the pacemaker in. At Columbia, approximately one-third of patients go home within 24 hours and the majority are home by 48 hours.
One aspect of the TAVR protocol Nazif believes is a good idea is the use of outpatient telemetry. In the new protocol, Schloss, Kereiakes, and colleagues recommend patients discharged with new conduction abnormalities but without a permanent pacemaker use the SEEQ Mobile Telemetry monitoring (Medtronic) or external cardiac ambulatory telemetry (ECAT). This would be managed by the cardiologist with an assist from the EP.
Competing Pressures
To TCTMD, Schloss noted there are competing pressures from the EPs who want to observe patients with hints of electrical conduction abnormalities and hospitals who want to see patients return home as soon as possible. Kereiakes agreed.
“We do feel the pressure, given the valve costs, to get patients out of the hospital,” said Kereiakes. “And also, a hospital is not a great place to be. It can be frustrating [for physicians] when you see a patient walking up and down the floor, but the QRS [has] widened, or the PR interval has widened, and they haven’t had any heart block. There’s no indication for a pacer and the patient wants to go home, but the EP guy says he wants to watch it for a day. It’s a struggle.”
With surgery, one of the historical advantages was long length of stay, with EPs under no pressure to remove the temporary pacemaker. Schloss said interventionalists “get it right most of the time,” but that the temporary pacing wire can be pulled too soon. Equally, he also thinks most are getting it right when it comes to implanting permanent pacemakers. The protocol has not been prospectively evaluated, nor have they assessed its impact on pacemaker implantation rates, he added.
“I think the protocol is more about tightening up all the efficiencies—that, to me, is a better goal,” said Schloss. The ultimate result of a streamlined approach would be a rational length of stay while preventing emergencies and unnecessary implantations. In other words, to not over- or undertreat TAVR patients.
“We can guess on this stuff, using basic principles of ECG management, and logic and commonsense, but unfortunately there’s exceptions to that and the exceptions can be pretty unpleasant,” said Schloss. “Also, none of this stuff has been studied—we’re going on instinct and experience. In 2017, that doesn’t really fly in medicine. We actually should have some real data, but it just hasn’t been accumulated at this point. We don’t have the quality evidence we need.”
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioDisclosures
- Schloss reports modest consulting relationships with Medtronic and Boston Scientific.
- Webb reports grant/research support and/or consulting for Edwards Lifesciences, Abbott, St. Jude Medical, Siemens Medical, and ViVitro.
- Nazif reports consulting for Edwards Lifesciences.
- Kereiakes report no conflicts of interest.


Comments