PROMISE Analysis Boosts Gatekeeper Role for FFRCT in Symptomatic Stable CAD
Calculating fractional flow reserve from coronary computed tomography results helps “address the weaknesses” of CTA alone, experts say.
Another analysis—this one from the PROMISE trial—supports a role for fractional flow reserve derived from computed tomography as a better gatekeeper than coronary CT angiography alone when it comes to determining which patients with stable chest pain should progress to invasive coronary angiography and which will ultimately need revascularization or have a cardiac event.
“FFRCT is really addressing a weakness of CT, in a sense,” lead author Michael Lu, MD (Massachusetts General Hospital, Boston, MA), told TCTMD. “One of the big downfalls of CT is that on CT, you see a lot more disease than you do on functional testing and as a result of that . . . there were about 50% more caths in the CT arm than in the functional arm in the [overall] PROMISE trial.”
As previously reported by TCTMD, the 10,000-patient PROMISE trial found that coronary CT angiography (CTA) as a first-line test did not yield better clinical outcomes than standard cardiac function tests—exercise ECG, nuclear stress tests, or stress echocardiography—among symptomatic patients at intermediate risk for CAD.
In the current study, published online before print today in JACC: Cardiovascular Imaging, investigators retrospectively calculated fractional flow reserve computed tomography (FFRCT) in PROMISE participants who had been randomized to coronary CTA and subsequently underwent intracoronary angiography (ICA) within 90 days, a total of 181 patients. FFRCT was deemed positive if < 0.80, and intracoronary angiography was deemed positive if lesions had a 50% or greater stenosis in the left main or 70% or greater in another coronary artery.
For the cohort as a whole, FFRCT results were discordant with a diagnosis of stenosis in just under one-third of both the CTA and ICA tests—a proportion similar to that seen in other studies comparing physiological and anatomical findings, Lu said.
In all, 91% of patients who underwent revascularization had FFRCT < 0.80. Compared with CTA alone, FFRCT proved better at identifying patients who subsequently went on to be revascularized or have a major adverse cardiac event (HR 4.3; 95% CI 2.4-8.9 vs HR 2.9; 95% CI 1.8-5.1; P = 0.033).
Extrapolating this further, said the authors, reserving ICA for patients with FFRCT < 0.80 would decrease the proportion of patients undergoing this invasive test by 44% and increase the proportion of patients receiving ICA who ultimately required subsequent revascularization by 24%.
The analysis, Lu and colleagues stress, can only be viewed as hypothesis generating. Importantly, PROMISE investigators were not privy to FFRCT results at the time of the trial. Rather, CTA results alone were guiding patient management. Moreover, Lu emphasized to TCTMD, PROMISE investigators were following Society of Cardiovascular Computed Tomography guidance for obtaining optimal CT images but were not given any forewarning that test results would be used to calculate FFRCT. They also received no feedback as to how to obtain images best suited to FFR calculations.
More Promise for CT With FFR Add-On
According to Lu, this PROMISE subanalysis reinforces results from the PLATFORM trial and, along with the overall PROMISE and SCOT-HEART trial results, helps establish CT as “a viable alternative” for the evaluation of stable chest pain. “And a major weakness of CT in those earlier trials is that it did send more patients to cath who probably don't need it,” he said. “FFRCT, I think, addresses that weakness in that it helps discriminate who actually needed the cath and who didn't.”
Indeed, commenting on the study for TCTMD, Matthew Budoff, MD (Los Angeles Biomedical Research Institute, Torrance, CA), agreed that coronary CTA still results in “unnecessary” angiograms.
“Using FFRCT, which requires no additional testing, . . . lowered the need for diagnostic catheterization by 44% in the current study and by 60% in the PLATFORM study [using] a European cohort,” Budoff said in an email. “Thus, using the full data available with coronary CTA (anatomy and FFR) will be the most cost-effective strategy for working up coronary artery disease and has already led to changes in international guidelines.”
Both Budoff and Lu cited a December 2016 update to the NICE guidelines in the United Kingdom, which now recommend CTA as a first-line test for patients with symptomatic stable chest pain. Moreover, both men noted, the NICE guidelines specifically call out FFRCT as “supported by the evidence,” to be used selectively as an add-on option that may reduce the need for invasive coronary angiography and revascularization.
FFRCT has no specific role in the current US guidelines, and for now the only Food and Drug Administration-approved method for calculating FFRCT is in the hands of a single company, HeartFlow, with a turnaround time that ranges from hours to days. Down the road, predicts Lu, the computational capacity to perform FFRCT will become much faster and, ideally, would be incorporated into CT scanners themselves.
Indeed, availability and accessibility of FFRCT were points also raised in an accompanying editorial by Subha V. Raman, MD, and Karolina M. Zareba, MD (Ohio State University, Columbus). “In an environment where only one vendor offers FFRCT analysis software approved for clinical use, centers can be charged significant per-case analysis or monthly license fees; such costs are not sustainable and limit adoption,” they write. Improvements to algorithms to broaden the patient population and enable faster turnaround times are also essential “to realize the promised clinical impact of FFRCT,” they conclude.
Lu also stressed that the role for FFRCT, at least for the time being, is as a gatekeeper in deciding whether a patient with stable CAD should proceed to cath, rather than as a means for decision-making during invasive procedures themselves.
“FFRCT is probably far from the point where it could replace FFR or iFR in patients in whom you're trying to decide whether they need a device,” he said. “I think if you're actually putting a device in, you would rely on the gold standard, FFR, and now some would argue iFR.”
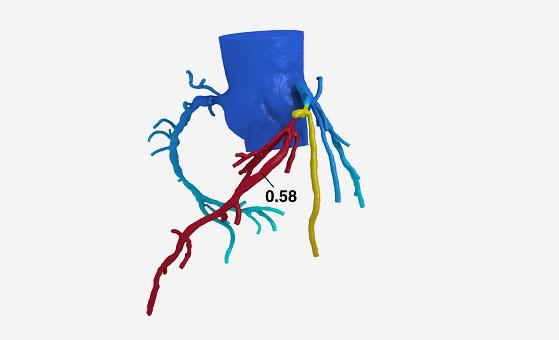
Photo Credit: HeartFlow Inc.
Shelley Wood was the Editor-in-Chief of TCTMD and the Editorial Director at the Cardiovascular Research Foundation (CRF) from October 2015…
Read Full BioSources
Lu MT, Ferencik M, Roberts RS, et al. Noninvasive fractional flow reserve derived from coronary CT angiography: management and outcomes in the PROMISE trial. J Am Coll Cardiol Img. 2017;Epub ahead of print.
Raman SV, Zareba KM. Coronary artery disease testing: Past, present, and future. J Am Coll Cardiol Img. 2017;Epub ahead of print.
Disclosures
- Lu reports support from an American Roentgen Ray Society Scholarship.
- Budoff reports consultant fees/honoraria from Janssen and Pfizer; research/grant support from General Electric; and serving on the speaker’s bureau for AstraZeneca.


Comments