Promising Preliminary Results for AccuCinch LV Restoration System in HFrEF
The main question to be addressed by the ongoing pivotal CORCINCH-HF trial is what this adds versus optimal GDMT alone.
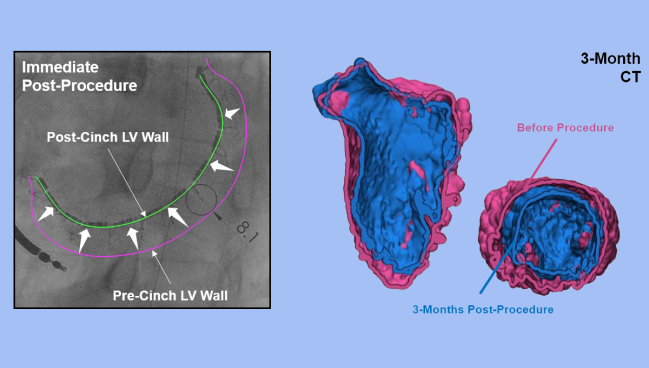
Photo Credit: Adapted from Jorde U. AccuCinch: outcomes of transcatheter lv volume reduction in HFrEF with a transcatheter ventricular restoration system. Presented at: THT 2023. Boston, MA.
BOSTON, MA—The investigational AccuCinch system (Ancora Heart) for transcatheter left ventricular restoration (TLVR) has a favorable safety profile and appears to improve echocardiographic endpoints and patient-centered outcomes in patients with heart failure with reduced ejection fraction (HFrEF) who remain symptomatic despite medical therapy, according to pooled data from multiple nonrandomized studies.
Patients who underwent the fully transcatheter procedure had a reduction in the size of the left ventricle, with signs of progressive reverse remodeling through a year of follow-up. There were also gains in LVEF, quality of life, and 6-minute walk test distance, as well as a reduction in NYHA class.
Nadira Hamid, MD (Allina Health Minneapolis Heart Institute, MN, and Cardiovascular Research Foundation, New York, NY), reported the findings here at the Technology and Heart Failure Therapeutics (THT) 2023 meeting. “Certainly this result is promising because with that change in LV end-diastolic volume [and] EF, you really see the quality-of-life improvement as well,” Hamid told TCTMD.
The results, published simultaneously online in the Journal of Cardiac Failure, also support a favorable safety profile, with few major adverse events related to the device or the procedure, she noted.
There’s a gap, Hamid said, in the treatment of patients with HFrEF and a dilated left ventricle who remain symptomatic despite use of optimal guideline-directed medical therapy (GDMT). If drugs fail, the eventual next step is advanced therapies like left ventricular assist devices (LVADs) and transplant. But a procedure like TLVR provides another option to patients, “giving them a chance before reaching the advanced heart failure therapies to improve their quality of life and overall outcomes,” Hamid said.
Of note, prior attempts at ventricular reconstruction in patients with dilated cardiomyopathy, using either surgical or hybrid techniques, have managed to reduce ventricle size but have not improved hard events. Where the AccuCinch system might have an edge is in being fully percutaneous, thus potentially limiting any downsides from a safety perspective.
[It gives] them a chance before reaching the advanced heart failure therapies to improve their quality of life and overall outcomes. Nadira Hamid
Carlos Santos-Gallego, MD (Icahn School of Medicine at Mount Sinai, New York, NY), commenting for TCTMD, said the study is “very positive and very promising.” With this group of patients, who have a heavy comorbidity burden and high rates of mortality and hospitalization, “definitely there’s an unmet need there,” he said.
In addition to demonstrating the feasibility and the safety of the procedure, the study provides encouraging results regarding efficacy, he said, noting that drug therapies that have been shown to induce reverse remodeling also improve cardiac outcomes. He cited the angiotensin receptor-neprilysin inhibitor (ARNI) sacubitril/valsartan (Entresto; Novartis) and the sodium-glucose cotransporter 2 (SGLT2) inhibitors.
Still, the study is limited by the small sample size and the lack of randomization and blinding. All of those factors, he said, magnify the apparent benefits, which will likely be lessened in the ongoing CORCINCH-HF pivotal trial when the procedure is compared against GDMT. Moreover, LV function and volume were assessed using transthoracic echocardiography, which is noisier and less sensitive than cardiac MRI, Santos-Gallego said.
The population targeted in this study is undoubtedly underserved, he said, but with the introduction of quadruple GDMT, it will be a shrinking one. “From now on, we are preventing many patients from developing such an advanced stage of left ventricular remodeling, so in the future this device is definitely not going to be implanted in the majority of the population,” he said. “It’s going to be just for a very small percentage of the population, because luckily, fortunately, the rest of the patients are going to receive the benefits of the four pillars of treatment.”
The CORCINCH Studies
The AccuCinch device, delivered transfemorally, consists of several anchors placed on the inner wall of the left ventricle below the mitral annulus in a procedure that’s guided by fluoroscopy and echocardiography. The anchors are then cinched together, which shrinks the ventricle and reduce wall stress. The idea is that this will induce biological reverse remodeling and ultimately improve patient outcomes.
Hamid reported results from four single-arm CORCINCH studies of the system: three in the US and one in Europe. Of more than 100 patients treated across those studies, the current analysis included 51 patients (mean age 56 years; 86.3% men) with HFrEF and a dilated left ventricle who remained symptomatic (NYHA class II or higher) despite use of optimal medical therapy and who met two key inclusion criteria for the pivotal CORCINCH-HF trial: an LVEF of 20% to 40% and no significant mitral regurgitation (grade 2+ or less). All patients had an LV end-diastolic diameter of 55 mm or greater.
Dilated cardiomyopathy with ischemic etiology was observed in 25.5% of patients. Most (52.9%) did not have an implantable cardiac device, although 27.5% had an implantable cardioverter-defibrillator and 19.6% had a cardiac resynchronization therapy device.
More than half of participants (54%) were in NYHA class II, with 44% in class III and 2% in class IV. The mean LVEF at baseline was 29%. Mitral regurgitation was graded as none/trace in 33.3%, mild in 27.5%, mild-to-moderate in 19.6%, and moderate in 19.6%.
The median duration of the procedure was 131 minutes, and there were a median of 13 anchors placed. Median LV reduction with the cinching procedure was 9.3 mm as measured by fluoroscopy.
At baseline, the mean LV end-diastolic volume was 200.9 mL. Within a month of the procedure, this was reduced by an average of 11.3 mL, with further progressive reductions observed over the first year, suggesting the procedure induces biological reverse remodeling. The average reduction at 1 year was 33.6 mL.
There were gains in LVEF, as well, with a mean increase of 3.1% at 1 year.
Those changes were accompanied by a mean improvement in Kansas City Cardiomyopathy Questionnaire (KCCQ) overall score of 12.0 points at 1 month, which was sustained at 1 year (improvement of 16.4 points). There was also an increase in 6-minute walk test distance, by an average of 45.9 meters at 1 year.
Roughly two-thirds of patients improved their NYHA class by at least one class, with 94% either improved or unchanged. At 1 year, 90% of patients were in NYHA class I or II, up from 54% at baseline (all NYHA class II).
All of those results were observed on the background of unchanged medical therapy, Hamid noted. At baseline, 90% of patients were on beta-blockers, 78% on a mineralocorticoid receptor antagonist (MRA), 63% on an ARNI, and 27% on an ACE inhibitor or ARB. The studies were conducted before SGLT2 inhibitors were considered part of GDMT for heart failure.
The safety profile was favorable, with a low rate of device- or femoral artery access-related major adverse events through 1 year, Hamid reported. There was one stroke possibly related to the device and one small pericardial effusion that was definitely related, but there no deaths or MIs. There were three adverse events related to arterial access that all resolved without sequelae, Hamid said.
Lingering Questions
What the results of the procedure will look like on top of and compared with current, quadruple GDMT that includes an SGLT2 inhibitor remains unclear, and the ongoing CORCINCH-HF pivotal trial will provide insights.
Santos-Gallego pointed out that medical therapies, and SGLT2 inhibitors in particular, have been shown to shrink LV volumes on their own. He cited the single-center EMPATROPISM trial, in which empagliflozin (Jardiance; Boehringer Ingelheim/Eli Lilly) provided a greater reduction in LV end-diastolic volume than did placebo (-25.1 vs -1.5 mL).
Even on best GDMT, however, a small percentage patients will remain symptomatic and progress, presenting an opportunity for interventions like TLVR with the AccuCinch system, Santos-Gallego indicated. Unlike prior attempts at ventricular restoration, this one is less invasive and does not create a massive restriction on the left ventricle, as was seen with prior surgical methods, he added.
“It’s a very promising study for a small percentage of patients who are clearly an unmet need,” he concluded.
As for where this might fit into the management of patients with HFrEF if it gains regulatory approval, Hamid noted that the population of such patients is expected to grow in the coming years, which will bring additional costs to the healthcare system. “Hopefully with this intervention we can help reduce that cost overall and the need for the advanced therapies of LVAD or heart transplantation,” she said. “That’s why there’s this gap I think that this therapy would fit in really nicely.”
It’s just this vicious cycle where the mitral valve starts leaking more, the left atrium gets bigger, and the right side of the heart starts getting worse. So if [TLVR] can stop that part of the cycle of the enlargement, then that is encouraging. Mackram Eleid
Mackram Eleid, MD (Mayo Clinic, Rochester, MN), who was not involved in the study, said these data indicate that the AccuCinch system is safe and effectively reduces the size of the left ventricle, which is encouraging because a dilated left ventricle causes other problems. “It’s just this vicious cycle where the mitral valve starts leaking more, the left atrium gets bigger, and the right side of the heart starts getting worse. So if [TLVR] can stop that part of the cycle of the enlargement, then that is encouraging.”
Eleid said he didn’t put too much weight into the other outcome findings because there was no control group, although he added that the level of reduction in LV volume observed here would be expected to reduce endpoints like death and hospitalization.
Even so, the pivotal trial will provide a more-definitive answer. “It’s not actually fixing the problem of the muscle of the heart. It’s just kind of cinching it up,” Eleid said. “So I think that’s why it remains to be seen how much benefit patients would actually have from that.”
Like Hamid, he noted that some patients remain in need of additional treatments even on GDMT: “At some point the medical therapy reaches its limit of benefit, so I still think there’s a potential role for things like this.”
The AccuCinch device is not the only transcatheter option being developed to repair the left ventricle in patients with HFrEF. At THT, Gregg Stone, MD (Icahn School of Medicine at Mount Sinai, New York, NY), reported data on the ongoing first-in-human experience with the V-sling device (Cardiac Success), based on earlier surgical techniques for papillary muscle approximation to reshape the ventricle. The transcatheter approach comes with the “potential to treat all heart failure due to dilated cardiomyopathy with or without mitral regurgitation,” Stone said, noting that the device does not block future interventions.
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Hamid N. Transcatheter left ventricular restoration in patients with heart failure. Presented at: THT 2023. March 21, 2023. Boston, MA.
Stone G. A left ventricular transcatheter repair device for HFrEF patients: FIH experience with the Vsling device. Presented at: THT 2023. March 21, 2023. Boston, MA.
Disclosures
- Hamid, Eleid, and Santos-Gallego report no relevant conflicts of interest.





Comments