Prosthesis-Patient Mismatch After Aortic Valve Replacement Declining but Tied to Poorer Survival
Surgeons should be comfortable performing a variety of techniques that are required to minimize PPM, one expert says.
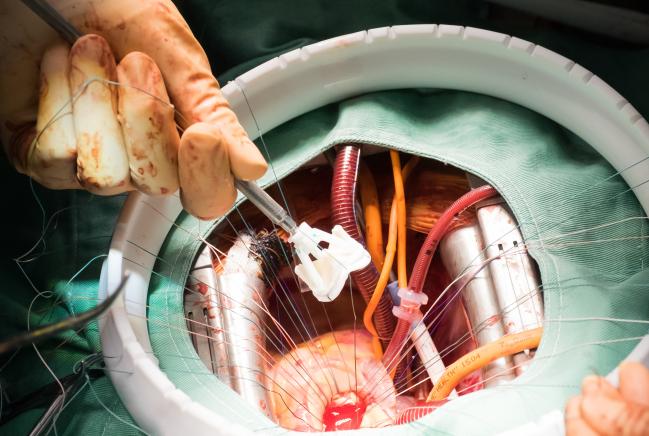
Prosthesis-patient mismatch (PPM) after surgical aortic valve replacement has become less common over time, but it remains associated with worsened clinical outcomes, a new study shows. Also, a second analysis indicates that annular size is related to hemodynamic measures and PPM in patients undergoing either transcatheter or surgical AVR.
In the first study, led by John Fallon, MD (Dartmouth-Hitchcock Medical Center, Lebanon, NH), both moderate and severe PPM after surgical AVR were associated with lower survival through 10 years of follow-up and higher rates of readmission for heart failure and redo valve procedures. And in the second, led by G. Michael Deeb, MD (University of Michigan, Ann Arbor), PPM was less frequent with TAVR versus surgery in patients with small or medium annuli, with no difference in patients with larger annuli.
Both studies were presented at the Society of Thoracic Surgeons (STS) meeting in Houston, TX.
Negative Impact of PPM
The clinical significance of PPM has remained unclear, according to Fallon, because prior studies exploring the issue have used a variety of ways of measuring effective orifice area and have included data from single centers only. Thus, he told TCTMD, there was a need for a larger, definitive study.
He and his colleagues looked at data from the STS Adult Cardiac Surgery Database on 59,779 patients 65 years or older who underwent isolated surgical AVR between 2004 and 2014. That information was linked to Medicare claims data.
The researchers divided patients into three groups based on the degree of PPM, which was calculated by dividing the effective orifice areas of various valve types by body surface area:
- None: > 0.85 cm2/m2 (35%)
- Moderate: ≤ 0.85 to ≥ 0.65 cm2/m2 (54%)
- Severe: < 0.65 cm2/m2 (11%)
Through 10 years of follow-up, the rate of readmission for congestive heart failure was lowest in patients without PPM (17%), increasing to 20% and 22% in those with moderate and severe PPM, respectively (P < 0.001). The rates of redo AVR were 1.2%, 1.9%, and 3.0% across groups (P < 0.001).
Moreover, 10-year adjusted survival rates were 46%, 43%, and 35% going from no to severe PPM (P < 0.001). Survival was impaired with both moderate and severe PPM, and Fallon said the relationship with moderate PPM has not been shown before.
The good news, he said, is that the rate of moderate PPM declined by a relative 22% (from 60.1% to 46.8%) and the rate of severe PPM dropped by a relative 55% (from 13.8% to 6.2%) during the study period.
Nevertheless, there remains room for improvement. Fallon noted in his presentation that about 90% of all PPM cases were in patients receiving valves with diameters of 23 mm or less. “Surgeons should be aware that small valves, especially 19s and 21s, are associated with poorer outcomes, plain and simple,” he said.
He added that consideration of avoiding PPM should become an important part of preoperative planning, an idea he credited to Philippe Pibarot, DVM, PhD (Québec Heart and Lung Institute and Laval University, Quebec, Canada). Using an effective orifice area reference chart and a patient’s body surface area, surgeons can decide on the minimum valve size needed to avoid PPM before the procedure, he said.
The next logical research question, Fallon said, is whether annular enlargement to allow implantation of a larger valve has an effect on outcomes.
Annular Size and PPM
In the other PPM study, Deeb and colleagues investigated the relationship between annular size and hemodynamics and the incidence of PPM (< 0.85 cm2/m2) after either TAVR with the self-expanding CoreValve prosthesis (Medtronic) or surgical AVR using data from the high-risk cohort of the CoreValve US Pivotal Trial.
The frequency of PPM was associated with annular size in the surgical patients only, increasing from 39.0% in patients with large annuli to 53.2% in those with medium annuli to 66.7% in those with small annuli. TAVR was associated with lower rates of PPM compared with surgery in patients with small and medium annuli (30.0% and 22.4%, respectively), with no difference based on AVR type in patients with large annuli.
In terms of hemodynamics, mean aortic valve gradients were lower in patients with small and medium annuli undergoing TAVR versus surgery at all time points up to 2 years after the procedures. Gradients increased as annular size decreased in the surgical group, but gradients were similar across annular sizes in the TAVR group.
“TAVR results in better hemodynamics and less PPM and should be strongly considered when choosing a valve for small and medium size annuli,” the investigators write.
Reducing PPM
Vinod Thourani, MD (Emory University, Atlanta, GA), a member of the STS board of directors, commented to TCTMD that there has been a belief that surgeons have not been putting in large enough valves, although there have been “mixed reviews” on whether PPM is clinically important.
Fallon’s study shows that PPM does, in fact, negatively affect outcomes, Thourani said, while also demonstrating that PPM is becoming less of a problem.
“It shows that the surgical community is responding to the notion that PPM is not good,” he said, noting, however, that severe PPM still occurs in about 6% of patients. The study “should prompt people to start thinking about it more, if they haven’t already.”
Thourani said there are four main ways to reduce the occurrence of PPM: careful selection of valve type, use of stented versus stentless valves, root replacement, and root enlargement. “Surgeons should be comfortable in doing a variety of techniques that are required to minimize PPM,” he advised.
In regard to Deeb’s study, Thourani noted that the investigators did not look at moderate and severe PPM separately; doing so might have provided different results.
The overall message from the two studies, he said, is that “the heart team should assess these patients to make decisions on what they think is best. We think that having a lower gradient is better and that having those four techniques for a way to minimize severe PPM is an important adjunct.”
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Fallon JM, DeSimone J, O’Brien S, et al. Incidence and consequence of patient-prosthesis mismatch after surgical aortic valve replacement: an analysis of the STS Adult Cardiac Surgery Database. Presented at: Society of Thoracic Surgeons Meeting 2017. January 23, 2017. Houston, TX.
Deeb G, Chetcuti S, Yakubov S, et al. Impact of annular size on hemodynamics and incidence of prosthesis-patient mismatch following surgical aortic valve replacement or transcatheter aortic valve replacement with a self-expanding bioprosthesis. Presented at: Society of Thoracic Surgeons Meeting 2017. January 24, 2017. Houston, TX.
Disclosures
- Fallon and Deeb report no relevant conflicts of interest.
- Thourani reports receiving research funding from Edwards Lifesciences and Medtronic and serving as a consultant to Edwards Lifesciences.


Comments