Quantitative Flow Ratio Shows Potential in Cath Lab
The FAVOR II studies open the door to an angiography-based strategy of assessing hemodynamically significant stenosis.
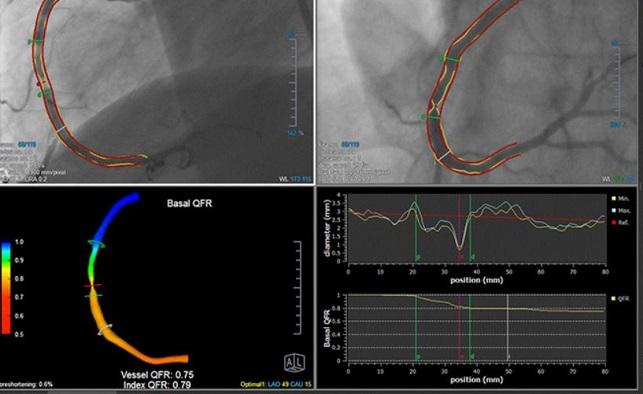
DENVER, CO—A novel angiography-based method for deriving fractional flow reserve (FFR), assessed online in the cath lab without pressure wires or induction of hyperemia, appears feasible and able to accurately detect functionally significant coronary lesions.
Accuracy of the method, known as quantitative flow ratio (QFR), was investigated in the FAVOR II China and FAVOR II Europe-Japan studies, which were presented in a First Report Investigations session. QFR is an estimate of FFR based on fluid dynamic equations and emulated hyperemic flow velocity. It is computed from lumen contours in two standard angiographic projections, and contrast flow velocity is estimated by frame count during baseline conditions. The image runs are then transferred by local network to the QFR system.
“Angiography-based functional lesion evaluation may appear as a cost-saving alternative to pressure wire-based assessment,” said presenter Jelmer Westra, MD (Aarhus University Hospital, Denmark).
FAVOR II China
In FAVOR II China, published simultaneously in the Journal of the American College of Cardiology, vessel-level diagnostic accuracy of QFR in identifying hemodynamically-significant coronary stenosis was 97.7% and patient-level diagnostic accuracy was 92.4% (P < 0.001 for both), according to Bo Xu, MBBS (Fu Wai Hospital, Beijing, China).
The prospective, multicenter trial enrolled 308 consecutive patients at five centers in China in June and July 2017. Eligible patients had at least one lesion with diameter stenosis of 30% to 90% and reference diameter 2 mm or greater by visual estimation. In this study, QFR (AngioPlus, Pulse Medical Imaging Technology, Shanghai, China), quantitative coronary angiography (QCA), and FFR (reference standard ≤ 0.80) were assessed online in a blinded fashion during coronary angiography, then reanalyzed offline in an independent core lab. In total, online QFR and FFR results were obtained in 328 of 332 vessels.
In other results, QFR showed superior sensitivity and specificity compared with QCA: 94.6% vs 62.5% and 91.7% vs 58.1% (P < 0.001 for both).
These data demonstrate “clinical utility of QFR for use in diagnostic catheterization laboratories,” Xu said.
FAVOR II Europe-Japan
QFR also showed superior sensitivity and specificity in comparison to 2-D QCA with FFR as the gold standard in FAVOR II Europe-Japan: 88% vs 46% and 88% vs 77% (P < 0.001 for both). The overall diagnostic accuracy of QFR was 88%. When the researchers analyzed feasibility per vessel, the rate of successful QFR computations in attempted cases was 97%.
The observational study enrolled 272 patients with the same angiographic inclusion criteria as FAVOR II China at 11 centers in Europe and Japan from March to October 2017.
Westra and colleagues also looked at results of the QFR-FFR hybrid approach. “Assuming that FFR is required in the diagnostic gray zone of QFR, pressure wire-free assessment is possible in potentially 68% of all lesions while ensuring more than 95% accuracy,” he said. The same was observed in FAVOR II China.
Taken Together
This new diagnostic approach could also potentially save time in the cath lab. The mean time for QFR assessment was 4.36 minutes in FAVOR II China and 4.8 minutes in FAVOR II Europe-Japan, compared with 7 minutes for FFR.
Both Xu and Westra concluded that the next step is adequately powered randomized trials comparing clinical outcomes with QFR versus standard diagnostic strategies.
During a discussion, panel members deliberated whether a study of clinical outcomes is required.
Alexandra J. Lansky, MD (Yale School of Medicine, New Haven, CT), referred to QFR as a “somewhat disruptive” technology. “It really can be used in all cath labs,” she said, noting that QFR “takes away all the complications associated with invasive FFR assessment. . . . We have very consistent results here with very high accuracy. Do we need to go to clinical outcomes?”
However, Gary S. Mintz, MD (Cardiovascular Research Foundation, New York, NY), pointed to questions about the potential for bias and overall generalizability, the need for a technician, and comparisons to previously seen limitations of online QCA. “It may be possible to improve the [QFR] algorithm so that it becomes automated,” he said, adding, “Reproducibility is important.”
Photo Credit: Medis Suite
Sources
Xu B. FAVOR II China: Diagnostic accuracy of the angiographic quantitative flow ratio in patients with coronary artery disease. Presented at: TCT 2017. October 31, 2017. Denver, CO.
Westra J. FAVOR II Europe Japan: Diagnostic Accuracy of the Angiographic Quantitative Flow Ratio in Patients With Coronary Artery Disease. October 31, 2017. Denver, CO.
Disclosures
- Westra reports receiving grant/research support and consulting fees/honoraria from Medis Medical Imaging Systems bv.
- Lansky and Xu report no relevant conflicts of interest.
- Mintz reports receiving grant support/research contracts from Boston Scientific, St. Jude Medical and Volcano Corporation and consulting fees/honoraria/speakers bureau for Acist, Boston Scientific and InfraRedX.
Comments