Restarting Oral Anticoagulation After Intracerebral Hemorrhage Tied to Better Outcomes
Resuming therapy was associated with lower risks of mortality and ischemic stroke and increased odds of a favorable functional outcome.
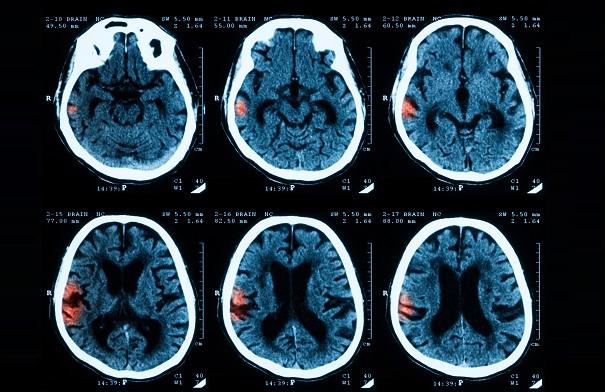
HOUSTON, TX—Patients who have an intracerebral hemorrhage (ICH) while taking oral anticoagulation for the prevention of stroke related to A-fib fare better over the next year if they reinitiate treatment, a meta-analysis shows.
Resumption was associated with better outcomes without an increase in the risk of recurrent ICH, regardless of whether patients had lobar or nonlobar hemorrhages, Alessandro Biffi, MD (Massachusetts General Hospital, Boston), reported here at the International Stroke Conference.
“These findings do support the need for clinical trials of oral anticoagulation resumption,” he said at a press conference.
Mark Alberts, MD (Hartford Hospital, CT), an American Stroke Association spokesperson, agreed, saying that the decision regarding restarting oral anticoagulation after ICH “is one of the most vexing issues in vascular neurology nowadays.” He noted that as the population ages, there will be more people with A-fib and thus higher numbers of both ischemic and hemorrhagic strokes in the setting of A-fib.
Few patients in the current analysis were taking non-vitamin K antagonist oral anticoagulants (NOACs), and Alberts said that introduction of those newer agents “is a huge game changer because the one thing that we can all agree on is that . . . the NOACs do have a reduced risk of cerebral hemorrhage compared to warfarin, or the vitamin K antagonists [VKAs].”
Pointing out that observational analyses like Biffi’s suffer from ascertainment bias, Alberts said, “We need data from prospective, randomized trials to figure out what the best approach is going forward.”
Resumption Varies Across Centers
Biffi said that whether to resume oral anticoagulation after ICH is a major clinical dilemma. It is commonly encountered, he said, because 10% to 15% of all ICHs occur in patients who are taking oral anticoagulation. Prior studies exploring reinitiation of therapy have not delved into potential differences based on ICH location—ie, lobar or nonlobar. That’s an important distinction, Biffi explained, because lobar hemorrhages are more closely related to cerebral amyloid angiopathy and nonlobar hemorrhages are more directly related to hypertensive small-vessel disease; lobar hemorrhages also carry a higher risk of recurrence.
The meta-analysis included individual patient-level data from three studies: the multicenter RETRACE study from Germany (542 patients), a longitudinal Mass General study (268 patients), and the multicenter ERICH study from the United States (217 patients). All patients had a first acute ICH confirmed by CT while taking oral anticoagulation; less than 5% were taking a NOAC.
Across the studies, 15% to 46% of patients resumed anticoagulation after ICH. Through the first year of follow-up, 39% to 52% had a favorable functional outcome (modified Rankin Scale score 0 to 3), 22% to 37% died, 3% to 7% had a recurrent ICH, and 5% to 11% had an ischemic stroke.
In patients with nonlobar ICH, reinitiation of anticoagulation was associated with reductions in the following outcomes:
- Mortality (HR 0.26; 95% CI 0.17-0.39)
- All-cause stroke (HR 0.45; 95% CI 0.28-0.71)
- Ischemic stroke (HR 0.42; 95% CI 0.22-0.81)
There was also a greater chance of achieving a favorable outcome (HR 4.41; 95% CI 2.92-6.67), without an increase in the risk of recurrent ICH (HR 1.12; 95% CI 0.94-1.34).
The findings were similar for patients with lobar ICH.
Biffi noted that his team is still analyzing data to explore reasons behind restarting or withholding oral anticoagulation after ICH—practices that varied widely across centers in the three studies—but said that there is a clear association between greater severity of the initial ICH and a lower likelihood of reinitiation.
In addition, resumption rates were higher for patients with nonlobar ICH, which is consistent with evidence suggesting that the risk for recurrence is lower in this population, Biffi said.
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Biffi A. Resumption of oral anticoagulation after intracerebral hemorrhage is associated with decreased mortality and favorable functional outcome. Presented at: ISC 2017. February 23, 2017. Houston, TX.
Disclosures
- Biffi reports no relevant conflicts of interest.


Comments