RNA-Interference Agent Zilebesiran Looks Promising for BP: KARDIA-1
In the phase II dosing study, the injectable RNA-interference agent safely reduced ambulatory systolic BP through 6 months.
PHILADELPHIA, PA—Zilebesiran (Alnylam), an investigational therapeutic agent that interferes with messenger RNA to stop the production of angiotensinogen (AGT), lowers systolic blood pressure levels better than placebo in patients not on any other antihypertensive drugs, according to results from the phase II KARDIA-1 trial released Saturday.
AGT sits at the top of the renin-angiotensin-aldosterone system (RAAS), so blocking it has the potential to impact the body’s blood pressure regulation downstream.
The drug, given as single subcutaneous injections at 3- or 6-month intervals, produced stable “clinically meaningful and significant reductions” in 24-hour mean systolic BP, George Bakris, MD (University of Chicago, IL), reported at the American Heart Association (AHA) 2023 Scientific Sessions.
Moreover, he said at an AHA press briefing, zilebesiran demonstrated an “encouraging” safety profile in the study, with few adverse events and only mild or moderate drug-related adverse events with three different dosing regimens.
Zilebesiran “targets hepatic angiotensinogen synthesis,” Bakris explained. The idea in KARDIA-1 is that by reducing serum AGT levels, the agent would “result in a dose-dependent reduction of blood pressure that can be sustained over 24 weeks following a single dose.”
He summed up the mechanism for TCTMD. In short, said Bakris, “the liver is unable to make angiotensinogen, because it ‘blocks the recipe,’ if you will.” Other drugs also are targeting that protein, but through different means, he added.
Keith Ferdinand, MD (Tulane University, New Orleans, LA), who discussed the new results with the media, said that while zilebesiran is investigational and “not yet ready for prime time,” the KARDIA-1 trial “does suggest that now they can target the first step in the potent renin-angiotensin system, angiotensinogen, which then appears to lead to robust and continued blood pressure-lowering for up to 6 months.
“This may give the benefit of having an increase in adherence,” Ferdinand continued. “One of the problems with blood pressure medicines: after a year or so, only 50% of the patients continue to take [them]. If you increase adherence, you increase efficacy and perhaps you will protect against some of the target-organ damage in this group.”
KARDIA-1
KARDIA-1 enrolled 394 adults (mean age 57 years; 56% male; 25% Black; 6% Asian) whose daytime mean ambulatory systolic BP level was 135 to 160 mm Hg. Their 24-hour mean ambulatory BP at baseline was 141.8/81.8 mm Hg. Ninety percent had an eGFR ≥ 60 mL/min/1.73 m2, and slightly more than half were obese.
After a washout period of 2 to 4 weeks in which they stopped taking any prior antihypertensive drugs, the participants were randomly assigned 1:1:1:1:1 to receive subcutaneous injections of either placebo (every 3 months) or zilebesiran at doses of 150 mg (every 6 months), 300 mg (every 6 months), 300 mg (every 3 months), or 600 mg (every 6 months).
Overall, 92% of patients completed their assigned drug during the study’s double-blind period, with no differences among the four groups. A total of 17% of the zilebesiran group experienced a drug-related adverse event, though only 1% discontinued their drug due to an event. Injection-site reactions occurred in 6% and hyperkalemia in 5%. Other treatment-emergent adverse events with the agent were acute renal failure (1%), hepatic adverse events (3%), and hypotension (4%).
“The drug’s pretty well tolerated, with minimal side effects,” Bakris reported.
The mean reduction in serum AGT by 6 months was 88% for the 150-mg dose, with higher reductions of 93%, 98%, and 96% achieved with zilebesiran doses of 300 mg (6 months), 300 mg (3 months), and 600 mg, respectively.
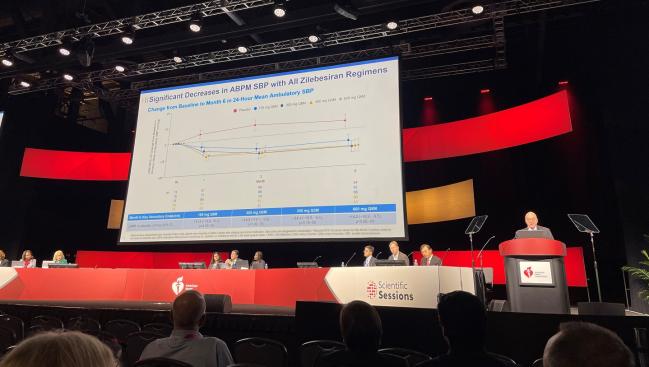
Bakris noted that these shifts correlated with decreases in systolic BP, seen at 3 months and then sustained through 6 months.
For mean 24-hour ambulatory systolic BP, the least-squares mean difference compared with placebo by 6 months was -11.1 mm Hg with 150 mg, -14.5 mm Hg with 300 mg (6 months), -14.1 mm Hg with 300 mg (3 months), and -14.2 mm Hg with 600 mg.
If you increase adherence, you increase efficacy and perhaps you will protect against some of the target-organ damage in this group. Keith Ferdinand
These results “support the potential for quarterly or biannual dosing of subcutaneous zilebesiran in achieving a consistent pharmacodynamic effect and effective blood pressure reduction through 6 months,” he concluded. “Zilebesiran is being further evaluated as an add-on therapy for the treatment of hypertension in the ongoing KARDIA-2 phase II study.
Sandra Taler, MD (Mayo Clinic, Rochester, MN), who moderated the press conference, noted that blocking AGT is merely “the first part of the chain,” which then has downstream effects. “This is starting right at the top. I guess the question would be: are there some negatives to that? Is there some harm in blocking that entire pathway from the start?”
“No, there’s no harm that’s been noted,” said Bakris.
Some experts at AHA raised the possibility that hyperkalemia could be a concern, but Bakris countered that this shouldn’t be the case if patients have normal kidney function or are monitored properly. Moreover, as with any drug targeting the RAAS system, it’s important for patients to remain hydrated by drinking enough water throughout the day, he advised.
In the late-breaking science session, discussant Anna F. Dominiczak, MD (University of Glasgow, Scotland), congratulated the research team, noting, “This is the first working successful antihypertensive in a number of decades.”
She agreed that the BP reductions seen with zilebesiran are consistent with the pharmacodynamic data showing AGT is decreased by more than 90%. Still, there are some clinical considerations, Dominiczak added. “I think it would be really interesting to measure other components of the [RAAS] system, the downstream molecular pathways.” The mild-to-moderate hyperkalemia seen in the study “is the evidence that things are happening downstream,” she noted.
Dominiczak suggested, too, that long-term follow-up could look into whether there’s a risk of refractory hypotension, not likely as a direct effect but rather as a consequence of RAAS inhibition under hemodynamic stress.
Caitlin E. Cox is Executive Editor of TCTMD and Associate Director, Editorial Content at the Cardiovascular Research Foundation. She produces the…
Read Full BioSources
Bakris G. Sustained blood pressure reduction with the RNA interference therapeutic zilebesiran: primary results from KARDIA-1, a phase 2 study in patients with hypertension. Presented at: AHA 2023. November 11, 2023. Philadelphia, PA.
Disclosures
- Bakris has received consulting fees from Alnylam Pharmaceuticals, AstraZeneca, Bayer, GlaxoSmithKline, InREGEN, Ionis, Janssen, KBP Biosciences, and Novo Nordisk.





Comments