Short DAPT in High-Bleeding-Risk Patients Reduces Recurrent Events: MASTER DAPT
As patients experience all events, not just the first, researchers should consider adjusting their trials to capture all outcomes.
PARIS, France—One month of dual antiplatelet therapy (DAPT) after PCI using contemporary stents not only is associated with similar rates of adverse clinical outcomes compared with 3 months or more in patients at high bleeding risk, but also lowers the total number of events, according to new data from MASTER DAPT.
The substudy builds off the main paper, published in 2021 as the largest randomized trial in this space, which showed the noninferiority of a short course versus standard DAPT with regard to net adverse cardiac events (NACE), major adverse cardiovascular and cerebrovascular events, as well as less bleeding.
While the original study only included incident events, the new analysis, presented here at EuroPCR and simultaneously published online in the Journal of the American College of Cardiology, accounted for recurrent events as well.
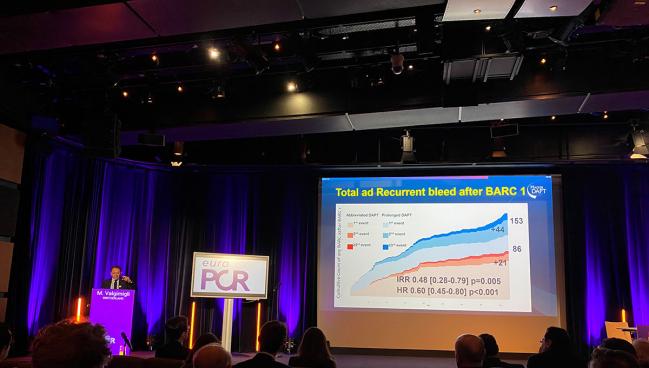
“We think that the assessment of total events confirms and potentially extends first event appraisal supporting abbreviated over standard DAPT duration with [high-bleeding-risk] patients included in the study,” said senior investigator Marco Valgimigli, MD, PhD (Cardiocentro Ticino Institute, Lugano, Switzerland), during the session.
Discussant Harlan M. Krumholz, MD (Yale New Haven Hospital, CT), who also serves as JACC’s editor-in-chief, said while some might argue that the new data simply confirm past evidence, the analysis is a “brilliant” and “important,” particularly for patients. “Patients experience the entire number of events and we need to be able to understand whether there's consistency if we consider all the events that occurred within the trial,” he said.
Moreover, the findings have implications for future clinical research, he argued.
“It’s statistically convenient to look at time-to-first-event, but that may not be the most patient-centric approach to how we should be thinking about the trials,” Krumholz said. “We shouldn't let statistical convenience dominate our thinking about what the right way is to be able to look at the entire burden of all of the events that occurred during the time of the trial.”
MASTER DAPT Substudy
For the new substudy, Dario Bongiovanni, MD, PhD (University Hospital Augsburg, Germany), Valgimigli, and colleagues looked at recurrent events in 4,579 patients randomized to abbreviated (median 34 days; n = 2,295) or prolonged DAPT (median 192 days; n = 2,284) in the MASTER DAPT trial.
Both the risks of NACE (214 events in 172 patients; HR 0.95; 95% CI 0.78-1.16) and MACCE (156 events in 138 patients; HR 0.96; 95% CI 0.76-1.29) over 355 days were similar with a shorter versus longer DAPT course. Patients receiving 1 month of DAPT reported fewer total major or clinically relevant nonmajor bleeding events (type 2, 3, or 5 BARC bleeding) than those taking at least 3 months of dual therapy (180 events in 148 patients; HR 0.78; 95% CI 0.64-0.94).
Abbreviated DAPT was also associated with significantly fewer total cerebrovascular accidents (34 events in 32 patients; HR 0.51; 95% CI 0.28-0.91) and total strokes compared with prolonged DAPT (25 events in 24 patients; HR 0.49; 95% CI 0.25-0.98).
Researchers say that bleeding is usually the “sentinel” event: roughly one in five MACCE events occurred following major/clinically relevant nonmajor bleeding, while about one in 25 had such bleeding followed a MACCE.
Notably, patients usually had their DAPT de-escalated following a BARC 2 but not BARC 1 event, but it was more frequently uptitrated in the short DAPT arm following an MI.
Don’t Write Off Even Minor Bleeds
During the discussion, session co-chair Davide Capodanno, MD, PhD (University of Catania, Italy), asked about the challenges of differentiating between BARC 1 and 2 bleeding events.
There is quite a “dichotomy” between the two, Valgimigli said, specifying that it’s more about how the patient and physician react to the bleed and not necessarily the severity of the event itself. “If you have the bleed and you as a patient decide not to do anything, not to seek medical attention, even for a massive bleeding, it remains BARC 1,” he explained. “If there is an action connected to the bleeding, that all of a sudden it becomes BARC 2.”
When bleeding receives any kind of medical attention, often physicians rethink the antiplatelet strategy and that triggers a change. “That's why after BARC 2, there was a big association with changing treatment” not seen with BARC 1, Valgimigli said. “In fact, our study confirmed a prior observation from the TRIUMPH registry, which showed that even BARC 1 . . . are a driver of recurrent bleeding events. If you start with an abbreviated DAPT to begin with, that risk is reduced. This is a very important observation, which, of course, has not been taken into account in the first time-to-event analysis because those events have been censored.”
Valgimigli further encouraged other researchers to change tacks from traditional methodology and take into account recurrent events as that would enable the field to “run more studies with less resources.”
As for being able to identify which patients might be more likely to suffer repeat events, Valgimigli stressed the value in not dismissing even a minor nosebleed. “Ask yourself the question whether you could, as a physician, do something to mitigate any recurrences, because the recurrences will be there and the fact that the patient had a minor bleeding event means that the patient is at a higher risk for a subsequent one,” he said.
Krumholz added that the response could mean DAPT de-escalation, but said there are other options available.
Valgimigli agreed, saying that switching to a less potent P2Y12 inhibitor like clopidogrel is valid, though not “very frequently pursued.”
Yael L. Maxwell is Senior Medical Journalist for TCTMD and Section Editor of TCTMD's Fellows Forum. She served as the inaugural…
Read Full BioSources
Bongiovanni D, Landi A, Frigoli E, et al. Recurrent events analysis of MASTER DAPT: total ischemic and bleeding events after abbreviated vs prolonged DAPT in HBR patient. J Am Coll Cardiol. 2025;Epub ahead of print.
Disclosures
- The MASTER DAPT trial is conducted with support from Terumo.
- Bongiovanni reports receiving grants and personal fees from Daiichi-Sanyko, Medtronic, Boston Scientific, Penumbra and Vesalio not related to the study.
- Valgimigli reports receiving grants and/or personal fees from Astra Zeneca, Terumo, Alvimedica/CID, Abbott Vascular, Daiichi Sankyo, Bayer, CoreFLOW, Idorsia Pharmaceuticals-Ltd, Universität Basel Department Klinische Forschung, Vifor, Bristol-Myers-Squib SA, Biotronik, Boston Scientific, Medtronic, Vesalio, Novartis, Chiesi, and PhaseBio.





Comments