ShortCut Leaflet Splitter Proves Safe, May Streamline Valve-in-Valve TAVI
The dedicated device can lacerate bioprosthetic leaflets poised to cause coronary obstruction—and does it quickly.
PARIS, France—A first-of-its-kind device used to slice through the leaflets of a failed bioprosthetic valve to forestall coronary artery obstruction during reintervention is safe and easy to use as an add-on during repeat valve procedures, the ShortCut study shows.
No patients died and only one disabling stroke occurred during the procedure, said lead investigator Danny Dvir, MD (Shaare Zedek Medical Center, Jerusalem, Israel), who presented the study here at EuroPCR 2024. He heralded the results as “better than expected.”
The ShortCut study, using the device of the same name made by PiCardia, is the pivotal trial required for US Food and Drug Administration approval as part of the agency’s breakthrough technology pathway, Dvir noted. The dedicated tool would replace the more technical, cumbersome, and higher-risk BASILICA procedure that had previously been the only established option for patients with failed surgical valves—and increasingly, failed TAVI devices—in whom a second procedure would likely end up obstructing the coronaries.
“Unfortunately, BASILICA is a long procedure. It's difficult to do and very difficult to teach,” Dvir said, adding that it takes on average 1 or even 2 hours to perform, even in expert hands. “For many, many centers across the world, the [BASILICA] procedure is difficult and long. For ShortCut, the average time for a single split was 27 minutes including TEE verification . . . , which is not required in clinical practice.” At his center, he can lacerate a leaflet using ShortCut in 10 to 15 minutes, he added. “I think that it's an easy add-on tool for our TAVR procedures.”
The study was published simultaneously in the European Heart Journal.
Getting Around a Problem
The catheter-based device is advanced across the valve, positioned under fluoroscopy, and splits the target leaflet vertically from base to tip. If required, it can be repositioned to split a second leaflet (a “dual split”). After the ShortCut device is retrieved, the TAVI procedure can be done over the same guidewire.
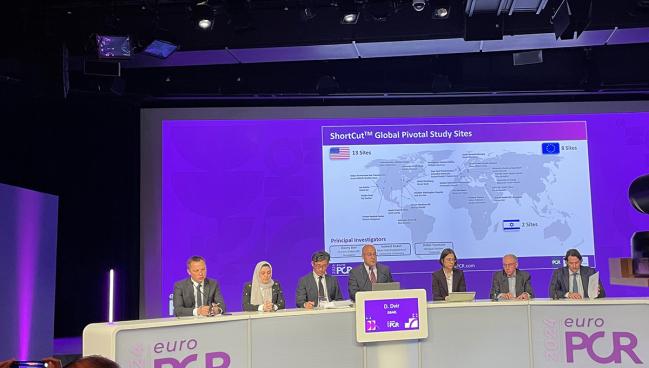
The ShortCut trial enrolled 66 patients at 22 sites: the patient number fell to 60 after withdrawals, deaths, or lack of consent before TAVI. All patients had risk factors for coronary ostium obstruction during a valve-in-valve procedure, including having low coronary height relative to the annular plane, narrow sinuses of Valsalva, short virtual transcatheter heart valve to coronary artery ostium distance, or short virtual transcatheter heart valve to sinotubular junction. Of note, fully 20 of the 22 participating sites had not used the device before trial participation.
Successful leaflet splitting, the trial’s primary endpoint, was accomplished in all first attempts; a dual split was deemed necessary in 36.7% of procedures. Freedom from the primary safety endpoints of mortality or stroke related to the procedure or device at 7 days or hospital discharge was achieved in all but one patient, who suffered a disabling stroke at day 4. Two patients died within 30 days of noncardiac causes, two patients with known renal impairment required temporary dialysis, and one patient had cardiac tamponade caused by the guidewire positioning.
After TAVI, all but three patients had unobstructed coronary access—in the three remaining patients, access was managed with coronary stents. Asked about those patients following his presentation, Dvir said he was unsurprised and unconcerned.
“In all of our attempts to prevent coronary obstruction, there will still be some cases with coronary obstruction, it’s part of life,” said Dvir. “The really important question is not whether there was coronary obstruction, it's whether the patient was affected poorly because of the event.” Here, the complication was swiftly managed, he said. “If we are able to treat that condition quickly, without having a real adverse event, then I'm not really [worried].”
Prediction the Future
During a press conference discussing the device, Dvir said he had no insights into what the cost of the device would be, assuming approval, but countered that BASILICA, too, carries a significant price tag. “How do we quantify the cost of having a safe procedure? What will be the cost of having a patient that will have coronary obstruction, the hospital stay, the potential death of a patient?”
Alternatively, he continued, what is the cost of telling a patient with a failed bioprosthetic that they are too high risk to get a repeat intervention—medical therapy also has costs, as does sending a complex patient for surgery. “All of these considerations are expensive indirectly,” Dvir countered.
Philippe Généreux, MD (Morristown Medical Center, NJ), a co-investigator on the study, commented on the cost question for TCTMD. This isn’t a device that is “nice to have,” he insisted, but rather a prerequisite for a significant number of patients. Currently, valve-in-valve procedures make up around 7% of his weekly TAVI caseload: he predicts that to double in the next 10 years. He estimates that fully 50% of those redo patients will face risks for coronary obstruction.
“I believe the price of the device by itself will not be prohibitive given the extremely needed nature of this device for a subset of patients that are very challenging and complex, and that we cannot address with current devices,” Généreux said.
Commenting on ShortCut for TCTMD, Marco Barbanti, MD (Ferrarotto Hospital, University of Catania, Italy), who was not involved in the trial and has not used the device himself, also estimated the proportion of redo patients at risk to be in the range of 44-50%, particularly for self-expanding TAVI devices. Coronary obstruction, he stressed, is a “life-threatening” complication.
“At the moment, this is a technology that needs to be developed because in the future we’re going to see a lot of patients with degenerated transcatheter valves,” Barbanti said. In this analysis, just two patients had failed TAVI devices and the rest were failed surgical valves, but the TAVI number is swiftly rising.
“I think we’re going to see a pandemic in a few years, particularly if we’re treating patients age 65 and 70 years old, because they will come back . . . . I’m unbiased, but I think there is good reason for moving in this direction,” Barbanti added.
Généreux predicts leaflet modification—several other novel devices are also in development—is poised to open the field of TAVI in new ways, including native valve splitting in bicuspid disease and mitral valve disease, by permitting treatment of patients currently considered unsuited to transcatheter valve procedures.
Shelley Wood was the Editor-in-Chief of TCTMD and the Editorial Director at the Cardiovascular Research Foundation (CRF) from October 2015…
Read Full BioSources
Dvir D, Tchétché D, Leon MB, et al. Leaflet modification before transcatheter aortic valve implantation in patients at risk for coronary obstruction: the ShortCut study. Euro Heart J. 2024;Epub ahead of print.
Disclosures
- Dvir reports consulting for Edwards Lifesciences, Medtronic, Abbott, Haemonetics(OpSens), and Pi-Cardia.
- Généreux reports consulting for Edwards Lifesciences and PiCardia, and holding stock with PiCardia.
- Barbanti reports consulting for Boston Scientific, Edwards Lifesciences, and Medtronic.





Comments