STICH Myocardial Viability at 10 Years: Still No Link With CABG Effects
Viability testing continues to have a role as one factor of many that go into the decision to take a patient in for bypass surgery.
The presence of myocardial viability at baseline was not a predictor of the long-term mortality reduction attained with CABG in patients with ischemic cardiomyopathy in the STICH trial, even when follow-up was extended out to 10 years. Those findings mirror the conclusions reached at the 5-year mark, researchers report today.
As previously published, death from any cause occurred less frequently among patients with coronary disease and severe LV dysfunction who underwent CABG versus those among who received optimal medical therapy alone, a difference that reached statistical significance only after 10 years of follow-up in the STICHES extension study (58.9% vs 66.1%; P = 0.02).
An earlier publication at 5 years showed a similar trend, though the difference was not significant (36% vs 41%; P = 0.12). At that time, STICH researchers also observed that the presence of viable myocardium prior to surgery did not identify patients who were more likely to benefit from surgical revascularization.
Now, using the 10-year data, the investigators have come to the same conclusion they did 5 years earlier, as reported in a study published in the August 22, 2019, issue of the New England Journal of Medicine.
Still, Panza said, myocardial viability testing continues to have a role in the decision-making process around CABG.
“This is a very complex population of patients and the decision as to whether an individual patient should or should not undergo bypass surgery should not be based on the result of a single test—ie, a test of viability,” he said. “But the test of viability should be taken in the context of the coronary anatomy, the degree of left ventricular dysfunction, and the ability to do an effective bypass in the vessels that are stenotic and [are] supplying the dysfunctional myocardium. So there is a constellation of issues that are related to the decision, of which myocardial viability is merely one of them.”
James Udelson, MD (Tufts Medical Center, Boston, MA), who was not involved in the study, agreed, noting that there is a body of observational evidence to suggest that patients with—but not those without—viable myocardium benefit from revascularization. “What we see is that the surgeons still want this information to inform their decision,” he commented to TCTMD. “It doesn’t completely by itself drive the decision, but it’s a piece of information that they still feel is important.”
Why Doesn’t Myocardial Viability Influence Outcomes?
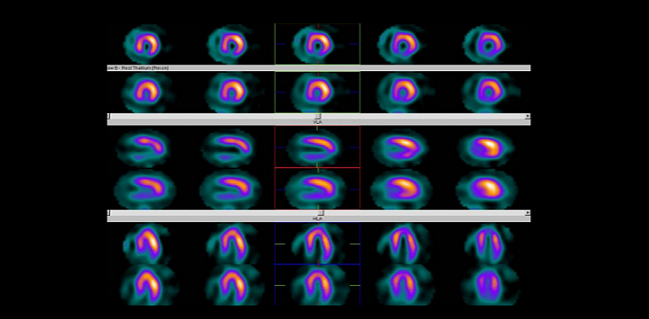
Of the 1,212 patients with CAD suitable for CABG and an LVEF of < 35% randomized in STICH, about half (49.6%) underwent a baseline assessment of myocardial viability using single-photon-emission CT, dobutamine echocardiography, or both. According to that testing, 81% of patients had viable myocardium and the rest did not.
There is a constellation of issues that are related to the decision, of which myocardial viability is merely one of them. Julio Panza
Within this viability substudy, CABG was associated with a lower risk of all-cause death through a median follow-up of 10.4 years when compared with medical therapy alone (62% vs 69%; adjusted HR 0.73; 95% CI 0.60-0.90), echoing what was seen in the overall trial.
Mortality risk was not significantly lower in patients with viable myocardium at baseline (64% vs 68%; HR 0.81; 95% CI, 0.63 to 1.03), and the presence of viability did not influence the treatment effect of CABG (P = 0.34 for interaction).
Both the authors and Udelson point out that there could in fact be a significant interaction, but that the number of patients without viable myocardium was too small to demonstrate it in this trial.
Udelson also explained that over time, noncardiovascular causes account for a greater proportion of deaths and the impact of any one factor at baseline—whether that’s myocardial viability, renal function, or ejection fraction—becomes diluted.
It’s unclear, Panza noted, whether the results would be the same if cardiac MRI were used to assess myocardial viability, the most common way of doing so in current practice. He said, however, that he doesn’t think this analysis’ findings are related to the precision of the tests used to identify viability.
LVEF Doesn’t Explain Mortality Benefit
The STICH investigators also looked into how myocardial viability was related to improvements in LVEF, and whether the latter were associated with long-term outcomes. They focused their analysis on 318 patients who had LVEF measured at baseline and 4 months later using the same modality.
LVEF increased in patients with—but not without—viable myocardium, regardless of whether they underwent CABG or received medical therapy alone. However, long-term risks of all-cause and CV mortality were not related to changes in LVEF, “suggesting that the mechanism of improvement in survival with bypass surgery is not related to the improvement in function,” Panza said, adding that it’s likely CABG is reducing mortality by preventing fatal MIs.
Udelson said the lack of a link between gains in LV function and reductions in long-term mortality after CABG is a bit unusual because interventions that improve ejection fraction tend to improve outcomes, at least in the heart failure literature. He pointed out, though, that a gain in LV function is only one of the good things that can happen after bypass surgery.
“Preventing myocardial infarction several years out is a really important mechanism of bypass surgery. Stabilizing what might be an arrhythmic substrate is another one,” he said. “So there’s a lot of mechanisms of benefit of bypass that don’t necessarily involve improving systolic function.”
Photo Credit: Siemens Healtineers
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Panza JA, Ellis AM, Al-Khalidi HR, et al. Myocardial viability and long-term outcomes in ischemic cardiomyopathy. N Engl J Med. 2019;381:739-748.
Disclosures
- STICH was supported by cooperative agreements with the National Heart, Lung, and Blood Institute. STICHES was supported by a separate grant from the National Institutes of Health.
- Panza and Udelson report no relevant conflicts of interest.


Comments