STROKE-VT: DOACs Cut Cerebrovascular Events After LV Arrhythmia Ablation
Despite some curious results, use of DOACs shortly after ablation “should probably make it into the guidelines,” one expert says.
In a finding that may improve the safety of an increasingly common procedure, use of direct oral anticoagulants (DOACs) instead of aspirin after radiofrequency ablation for ventricular tachycardia or premature ventricular contractions can reduce both clinical and subclinical cerebrovascular events, the STROKE-VT trial demonstrates.
DOAC-treated patients had lower rates of stroke (0 vs 6.5%) and TIA (4.9% vs 17.9%; P = 0.001 for both) in the first 30 days, as well as lower rates of MRI-detected asymptomatic lesions at both 24 hours (12.2% vs 22.8%; P = 0.03) and 30 days (6.5% vs 17.9%; P = 0.006), according to Dhanunjaya Lakkireddy, MD (Kansas City Heart Rhythm Institute and Research Foundation, Overland Park, KS).
There were no differences between the DOAC and aspirin groups in terms of in-hospital mortality (3.7% vs 2.7%; P = 0.73) or various types of bleeding, he reported during the Heart Rhythm Society (HRS) 2021 Scientific Sessions.
Another key finding was that retrograde aortic access, used in about 40% of patients overall, was independently associated with stroke/TIA (OR 2.60; 95% CI 1.06-6.37).
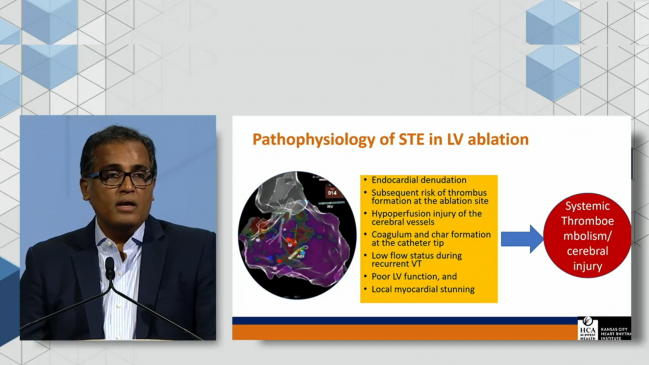
“So the take-home message from this particular study is that when we do the left ventricular ablations, I think it’s important to anticoagulate these people with a direct oral anticoagulant or an equivalent in order to mitigate the risk of systemic thromboembolic events,” Lakkireddy said at a media briefing, adding that “we should avoid a retrograde transaortic approach when it can be avoided.” He pointed out that prolonged ablation times and low ejection fractions were associated with increased risks as well.
Edward Gerstenfeld, MD (University of California, San Francisco), told TCTMD the trial results are relevant to any center performing ventricular tachycardia (VT) or premature ventricular contraction (PVC) ablations, noting that there is not a standardized approach to postprocedural antithrombotic therapy in this setting. Gerstenfeld said he’ll put patients on aspirin for a month after a typical VT or PVC ablation but use one of the DOACs to reduce the risk of thromboembolic events after more-extensive ablations. There are, however, no defined criteria guiding when to use aspirin versus oral anticoagulation.
The results for stroke and TIA were “pretty impressive in the degree of reduction,” said Gerstenfeld, associate editor of JACC: Clinical Electrophysiology, in which the STROKE-VT findings were simultaneously published. The reduction in subclinical lesions also was important, “although we know less about the relevance of these MRI-detected asymptomatic events.”
He raised questions about the high rate of stroke observed in STROKE-VT relative to prior studies and about how anticoagulation could have such dramatic effects when started several hours after the procedure. Nonetheless, he said, “the fact that they were able to get significant reductions in hard endpoints such as stroke and TIA is pretty striking, and I think it’s likely to change practice probably tomorrow.”
STROKE-VT
The number of VT ablations has increased around the world in recent decades, and risks of periprocedural systemic thromboembolic events and cerebral injury remain. There are, however, limited data on the optimal approach to antithrombotic therapy after ablations in the left ventricle, Lakkireddy said, noting that protocols have varied across existing studies.
STROKE-VT was designed to help fill that evidence gap. Investigators randomized 246 patients (mean age 60 years; 82.5% men) with ischemic or nonischemic cardiomyopathy to either a DOAC or aspirin starting 3 hours after postprocedural hemostasis was achieved. Mean ejection fraction at baseline was 33.4%.
About three-quarters of the patients underwent an ablation for VT, with the rest getting treated for PVCs. During the procedures, IV heparin was administered with activated clotting times kept above 350 seconds. DOAC-treated patients were more likely to undergo ablation for VT versus PVC and to be treated with amiodarone, and they had a greater total radiofrequency ablation time (2,095 vs 1,708 seconds). Retrograde access was more frequent in the aspirin group (45.5% vs 34.2%).
In addition to reductions in the proportions of patients with stroke, TIA, and MRI-detected lesions with DOAC therapy, there was also a reduction in the average number of MRI-detected intracranial lesions at 24 hours (1.2 vs 1.9; P = 0.02). That difference was no longer significant between 24 hours and 30 days (1.0 vs 1.2; P = 0.32), but the fact that there were still lesions detected at all “goes to tell you that there is a continued risk in these groups of people,” Lakkireddy said.
There was no difference in acute procedure-related complications between the DOAC and aspirin groups (12.2% vs 15.9%; P = 0.70).
When comparing outcomes between PVC and VT ablation, the researchers found no difference in the rate of stroke/TIA (16% vs 14%; P = 0.70), although MRI-detected lesion were more commonly found in the PVC group at 24 hours (25.8% vs 14.7%; P = 0.046). That’s possibly related to a greater need for retrograde aortic access, Lakkireddy said, “and that’s something that needs to be taken into consideration.” There was no longer a significant difference at 30 days, however (14.5% vs 11.4%; P = 0.52).
‘Guideline-Influencing’ Findings
Christine Albert, MD, (Smidt Heart Institute at Cedars-Sinai, Los Angeles, CA), who moderated the media briefing, noted, as Gerstenfeld and others did, that practice is variable when it comes to antithrombotic therapy after VT ablation. “This is really the first randomized trial data that I know of that we have on this, so I do think it will be guideline-influencing,” she said.
And Mina Chung, MD (Cleveland Clinic, OH), in comments following Lakkireddy’s presentation, took it a step further: “It’s a very important study, and I think that this could become our standard of care for managing anticoagulation after VTE and PVC left-sided ablations.”
For his part, Lakkireddy said, “I do believe this could be practice-changing,” adding that for left-sided ablations, “it is of paramount importance to anticoagulate these people for a short period of time, at least for 4 weeks.”
Gerstenfeld highlighted the high overall rates of stroke and TIA observed in STROKE-VT compared with other studies of VT ablation. “If I was a patient, that would make me kind of nervous about having a VT ablation, and it’s certainly higher than the incidence that we see in general practice.” That leads to questions about how the events were adjudicated and how severe they were, he said. The high rates could be due to closer follow-up compared with other studies, which the researchers themselves suggested, or to the nature of the procedures. The study investigators are “pretty well known as aggressive ablators,” Gerstenfeld said.
He also questioned why oral anticoagulation started hours after the procedure would provide such large reductions in events, which are thought to often occur in relation to dislodged atherosclerotic plaque during the ablation.
So the mechanism behind the observed benefit is unclear, “but the results do argue to give a DOAC for a month after PVC or VT ablation, and then if you have the option of a transseptal versus retrograde approach, it’s probably safer to use a transseptal approach,” Gerstenfeld said, adding that the findings regarding antithrombotic choice “should probably make it into the guidelines.” More information about the choice between transseptal and retrograde aortic access for LV ablation, he noted, will come from the ongoing TRAVERSE trial.
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Lakkireddy D, Shenthar J, Garg J, et al. Safety and efficacy of direct oral anticoagulant versus aspirin for reduction of risk of cerebrovascular events in patients undergoing ventricular tachycardia ablation (STROKE-VT). J Am Coll Cardiol EP. 2021;Epub ahead of print.
Disclosures
- Lakkireddy reports consulting for Abbott, Biosense Webster, Boston Scientific, Philips, Stereotaxis, and AtriCure Inc.Lakkireddy reports consulting for Abbott, Biosense Webster, Boston Scientific, Philips, Stereotaxis, and AtriCure Inc.





Comments