TEER May Surpass Medical Therapy in High-risk Atrial FMR Patients
Japanese registry data point to fewer deaths and heart failure hospitalizations, especially when MR is reduced to mild or less.
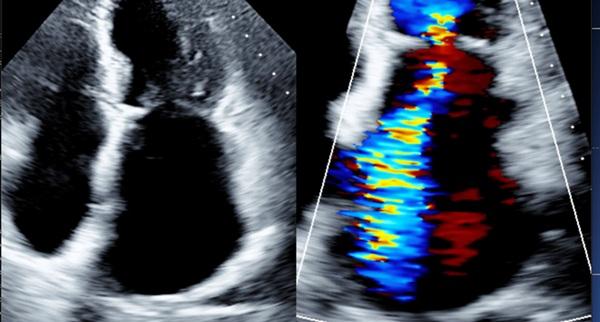
Photo Credit: Adapted from Asch FM. Atrial FMR primer: epidemiology, pathophysiology, imaging features, and clinical presentation. Presented at: TCT 2024. Washington, DC.
Patients with moderate or severe atrial functional mitral regurgitation (FMR) do better—with a lower likelihood of death and heart failure hospitalization—when they receive transcatheter edge-to-edge repair (TEER) rather than medical therapy, combined data from two real-world registries suggest.
Previously, the COAPT and RESHAPE-HF2 trials established TEER’s benefit in ventricular FMR, but “atrial FMR is a fundamentally different entity, both in mechanism and in left ventricular function,” Nobuyuki Kagiyama, MD (Juntendo University Graduate School of Medicine, Tokyo, Japan), the study’s corresponding author, told TCTMD. While distinct, the atrial etiology is less common and tends to be grouped together with other MR types, he said, so there’s a need for dedicated study of the condition, ideally through a randomized controlled trial.
But for now, the field relies on registry data, in this case from OCEAN-Mitral and REVEAL-AFMR.
“Our findings suggest that TEER may also confer meaningful benefit in atrial FMR, which is highly relevant for clinical practice,” Kagiyama wrote in an email. “The magnitude of the difference in all-cause mortality was particularly striking, even to us.” Thus, the intervention “could be considered a viable option for atrial FMR patients at high surgical risk, not only to improve symptoms but also potentially to extend survival,” he specified.
Heart failure specialist Akshay S. Desai, MD (Brigham and Women’s Hospital, Boston, MA), commenting on the new data for TCTMD, said atrial FMR “is increasingly recognized as an important consequence of . . . chronic atrial fibrillation. It’s a challenging problem. It tends to affect older patients. It tends to contribute to heart failure development, often in the setting of preserved ejection fraction. And it’s a context in which we don’t often have very effective or targeted medical therapy.”
These patients’ age along with the fact that they tend to have long-standing atrial fibrillation and heavy comorbidity burdens means many aren’t candidates for surgery, Desai added. “It’s an appealing group in which to consider a transcatheter approach if it modulates outcomes.”
In the absence of RCT data, it’s reassuring to see that among these selected patients undergoing TEER, MR was reduced to mild or less in nearly 80% of cases, he said. Still, real-world registries capture a “mixed bag” of patients and are “inherently vulnerable to a lot of residual confounding,” especially as it relates to the decision to perform TEER in some cases but not others.
Given these limitations, “I think this is likely to be an optimistic view of the potential treatment effect,” said Desai. “But it does give some security that, number one, we can do this and, number two, that there doesn’t appear, at least in this analysis, to be evidence of harm.”
Even with the caveats, “the study is provocative in that it suggests that there may be long-term treatment benefits that would support the use of this approach,” Desai said.
Led by Tomohiro Kaneko, MD (Juntendo University Graduate School of Medicine), the study was published online recently in the European Heart Journal.
OCEAN-Mitral and REVEAL-AFMR
Kaneko and colleagues compared data from two sources: 441 patients with moderate or severe atrial FMR treated by TEER (MitraClip; Abbott) who took part in the OCEAN-Mitral registry and 640 medically managed controls who participated in the REVEAL-AFMR registry. Mean age in the entire cohort was 80.1 years, and 60.5% were female. All participants were enrolled in Japan.
Procedural success was 95.2% in the TEER group, with 2.9% of patients experiencing a device-related complication (eight leaflet tears and five single-leaflet device attachments). Residual MR at discharge was mild or less for 78.3% of the TEER-treated patients, moderate for 18.9%, and moderate to severe or severe for 2.8%.
Compared with controls, the TEER group tended to be older (mean age 82 vs 79 years), had a higher prevalence of severe MR at baseline (49.7% vs 6.4%), were more likely to present with NYHA III or IV symptoms (57.4% vs 9.1%), and were more apt to have had a prior admission for heart failure (80.0% vs 24.5%). TEER-treated patients also were more often taking loop diuretics, tolvaptan, beta-blockers, and mineralocorticoid receptor antagonists at baseline.
The researchers, to account for these differences, performed overlap weighting based on propensity score, resulting in well-balanced characteristics between the two groups.
At 3 years, use of TEER was associated with lower risks of all-cause mortality and heart failure hospitalization, the study’s primary endpoint (HR 0.65; 95% CI 0.43-0.99), as well as all-cause mortality alone (HR 0.58; 95% CI 0.35-0.99).
At 1 year, the estimated incidence of the primary outcome was 12.3% with TEER and 21.7% with medical therapy. By 3 years, the difference became more pronounced, with rates of 21.0% and 44.3%, respectively. Exploratory analyses suggest the benefit of intervention was greater at 24 months in patients with mild or less residual MR after TEER (HR 0.49; 95% CI 0.30-0.81), whereas patients with worse levels of residual MR after TEER had outcomes similar to controls (HR 1.14; 95% CI 0.54-2.40).
Overall, the “findings suggest that TEER may provide clinically meaningful benefit in this older and frail patient population with limited treatment options,” they write. “Nevertheless, these results should be interpreted with caution due to the retrospective observational nature of the study, and prospective studies are warranted.”
The magnitude of the difference in all-cause mortality was particularly striking, even to us. Nobuyuki Kagiyama
Kagiyama pointed out that, prior to adjustment, TEER was most often used in patients with worse MR and more advanced heart failure. Propensity score-based analyses “substantially, though not completely, addressed these imbalances,” he acknowledged. “Factors not captured in the datasets—such as physical or social frailty—remain potential confounders, highlighting the need for prospective validation.”
For Desai, another missing bit of information is how contemporary medical therapy, particularly sodium-glucose cotransporter 2 inhibitors, might influence the findings, given that the REVEAL-AFMR cohort was enrolled in 2019 before these drugs were widely used. He also pointed out that the data may not be generalizable to patients outside of Japan.
Additionally, many patients in this study were at high surgical risk (median EuroSCORE 3.0), said Kagiyama. “For lower-risk patients, surgery—offering the possibility of concomitant tricuspid or atrial fibrillation procedures—may be preferable, but this warrants further investigation.”
When deciding between TEER and medical therapy for high-risk patients with atrial FMR, “selection should take into account MR severity, comorbidities, and left atrial size, aiming to intervene before extreme atrial enlargement develops,” he advised.
In practice, said Desai, “we would be considering [TEER] in patients who are failing standard medical therapy, understanding that there isn’t standard medical therapy for atrial functional MR per se. What we do have is medical therapy for heart failure.”
Thus, candidates for TEER would be patients with atrial FMR who have progressive heart failure symptoms while on appropriate medical therapy, are functionally limited, and are “of a mindset to be aggressive and open to the idea of a catheter-based intervention,” Desai explained. “I think if all those criteria are met, then that’s the population in which we consider this.”
Kagiyama said that, when TEER is being pursued, preprocedural echo assessment is an essential tool for identifying factors that predict procedural difficulty, such as atriogenic tethering or a low leaflet-to-annulus index. Such cases may warrant the implantation of multiple devices, he suggested, and should involve close collaboration between operators and echocardiographers.
Then, after TEER, “follow-up should include careful echocardiographic monitoring for residual MR, as our findings indicate that achieving and maintaining mild-or-less MR is key to long-term benefit,” he added.
Caitlin E. Cox is Executive Editor of TCTMD and Associate Director, Editorial Content at the Cardiovascular Research Foundation. She produces the…
Read Full BioSources
Kaneko T, Kagiyama N, Okazaki S, et al. Transcatheter edge-to-edge repair vs medical therapy in atrial functional mitral regurgitation: a propensity score-based comparison from the OCEAN-Mitral and REVEAL-AFMR registries. Eur Heart J. 2025;Epub ahead of print.
Disclosures
- Kaneko receives research grants from the Japanese Circulation Society and belongs to an endowed department funded by Abeam Consulting.
- Kagiyama receives research grants from AstraZeneca, EchoNous, and AMI; receives speaker honoraria from Eli Lilly, Novartis, Otsuka Pharmaceutical, Bristol Myers Squibb, and Boehringer-Ingelheim outside this work; and is affiliated with a department funded by Paramount Bed.
- Desai reports consulting for Endotronix, a subsidiary of Edwards Lifesciences, as well as for Abbott. He also has received research support from Abbott.




Comments