Tricuspid Interventions OK With Pacemakers, ICDs: TriValve Registry
A transcatheter fix may be reasonable in medically refractory TR, but teasing out the impact of meds and mitral repair will be key.
At experienced centers, the presence of a pacemaker or implantable cardioverter-defibrillator (ICD) lead going through the tricuspid valve should not preclude a transcatheter fix for tricuspid regurgitation (TR), data from the TriValve Registry suggest.
The presence of a cardiac electronic implantable device did not have a significant impact on how patients with severe symptomatic TR fared after a transcatheter procedure, either in the hospital or out to 1 year—reductions in TR, symptomatic improvements, and mortality rates were similar regardless of the presence of a device.
“The presence of a transtricuspid pacemaker lead per se does not increase the complexity of transcatheter tricuspid treatment with different devices, so we should not exclude patients from this kind of therapy just based on the presence of a pacemaker lead. And this is the first large series demonstrating this,” lead author Maurizio Taramasso, MD, PhD (University Hospital of Zurich, Switzerland), told TCTMD, noting that the procedures were performed at experienced centers and that it might be difficult to generalize the outcomes to a broader range of settings.
Erin Fender, MD (Christiana Care Health System, Newark, DE), who was not involved in the study, said the investigators explored an important question both because TR is highly prevalent in patients with intracardiac devices and because the devices themselves often preclude percutaneous treatment options.
“I think most of us practitioners are fairly reluctant to attempt intervention in that population because of concern for interaction with the intracardiac device lead,” Fender explained. “And so it’s a population of patients that’s historically been neglected in trials for these kinds of emerging therapies because of concern for those interactions.”
This new study, published online January 15, 2020, ahead of print in JACC: Cardiovascular Interventions, showed that performing a transcatheter fix for TR in patients with pacemakers or ICDs “was safe and feasible, and also suggested that it was clinically effective as well,” Fender said. “So it really provides reassurance to interventionalists working in this space that it’s reasonable to consider attempting one of these interventions in a patient with a device lead.”
TriValve Registry
Prior results from the TriValve Registry, including an analysis of 312 patients published a year ago, have suggested that various transcatheter approaches to fixing the tricuspid valve are feasible and safe and can improve clinical outcomes. But whether these procedures can be performed in patients with pacemaker or defibrillator leads remains a hot topic in the field, and the issue has not been examined in large-scale studies, Taramasso said.
This new analysis of TriValve Registry data, based on 470 patients with severe symptomatic tricuspid regurgitation (mean age 76 years; 62% women) treated at 21 centers in Europe and North America between 2015 and 2018, helps to fill that gap. About one-quarter of patients (25.7%) had a pacemaker or ICD with a lead through the tricuspid valve at the time of the transcatheter procedure.
Patients with an implanted device were more likely than those without a device to have NYHA class III/IV symptoms, ascites, and peripheral edema; more frequently had been admitted for an episode of right heart failure in the preceding year; and had higher levels of N-terminal pro–B-type natriuretic peptide. They had less-severe TR, as indicated by a lower effective regurgitant orifice area (0.6 vs 0.7 cm2; P = 0.02), but worse RV function.
Most of the tricuspid procedures were performed with the MitraClip (Abbott), with significantly greater use in patients with an implantable device (87.6% vs 76.5%; P = 0.03). The tricuspid intervention was done concomitantly with other valve procedures (nearly all involving MitraClip in the mitral position) in about one-third of cases.
Procedural success, defined as the patient surviving with successful transcatheter treatment with no more than 2+ residual TR, was achieved in about 80% of patients regardless of the presence of implantable device leads (P = 0.74). There were no differences between groups in periprocedural adverse events or in in-hospital mortality (3.7% in patients with implantable devices vs 2.9% in those without devices; P = 0.7). No cases of device dislodgement or malfunctioning were reported.
At 30 days, 73% of implantable-device patients and 70% of those without a device had residual TR graded 2+ or less (P = 0.6). Symptomatic improvement was seen in both groups, resulting in roughly two-thirds of patients in each group having NYHA class I/II symptoms at 30 days.
At 1 year, the survival rate was 73.6% in patients with a pacemaker or ICD and 80.7% in those without an implantable device, a nonsignificant difference (P = 0.3). The presence of a transtricuspid lead was not associated with mortality (HR 0.72; 95% CI 0.20-1.40).
Randomized Data Lacking
Fender, who co-authored an accompanying editorial with Chad Zack, MD (Penn State Health Milton S. Hershey Medical Center, Hershey, PA), pointed out that medical therapy, particularly intensive diuresis to address symptoms, remains the standard of care in patients with severe symptomatic tricuspid regurgitation. That doesn’t address the structural problem with the valve, however, “which is one of the attractive reasons to consider an intervention that actually alters the structure of the valve in a way that can reduce regurgitation. . . . Having a percutaneous intervention offers the possibility of actually fixing the valve itself, which may then reduce the need for symptomatic response with aggressive diuretics,” she explained.
I think we need controlled trials that account for the cotreatment of mitral disease and also for differences in medical therapy. Erin Fender
But there are no randomized data pitting transcatheter repair against optimal medical therapy in patients with severe symptomatic TR, Fender noted. RCTs are needed to help sort out questions regarding the impact of concomitant mitral regurgitation (MR)—which was more common in the patients with implantable devices in this study—and its treatment on the results of tricuspid intervention. She explained that much of the TR seen in these patients might be secondary to severe MR and that some of the reduction in TR could have been due to treating the MR.
Nevertheless, this study supports the use of transcatheter tricuspid repair in selected patients, Fender said.
“In a patient who has truly medically refractory symptoms, this study shows it is reasonable to consider and safe to consider this intervention, but I think right now there is insufficient evidence to say that this should be a widely applied therapy,” she said. “I think we need controlled trials that account for the cotreatment of mitral disease and also for differences in medical therapy. And until those studies are completed, there’s insufficient data to conclude that this is an appropriate stand-alone treatment for TR.”
Although its still early on in the development of transcatheter treatments for TR, Taramasso said, there is enough evidence from this and other studies to suggest that these procedures improve symptoms and may improve survival.
“All the signs tell us that we are doing something good for the patients,” he said. “Obviously, it’s a difficult technique, a difficult approach, and this should be centralized in highly experienced centers.”
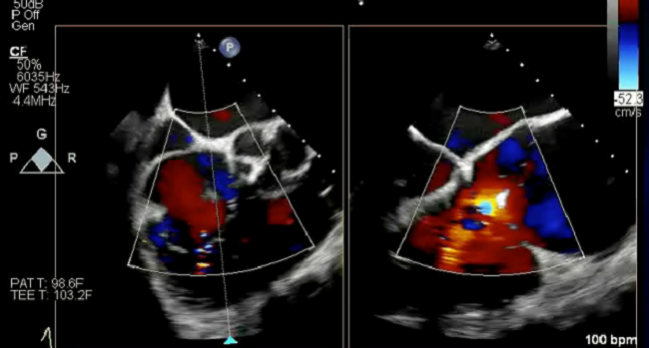
Photo Credit: Bae R. Step-by-step tricuspid clipping: echo and intervention working together. TCT 2018. September 28, 2019. San Francisco, CA.
Note: Several co-authors are faculty members of the Cardiovascular Research Foundation, the publisher of TCTMD.
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Taramasso M, Gavazzoni M, Pozzoli A, et al. Outcomes of transcatheter tricuspid valve intervention in patients with pacemaker or defibrillator leads: data from the TriValve Registry. J Am Coll Cardiol Intv. 2020;Epub ahead of print.
Fender EA, Zack CJ. Moving the bar for transcatheter tricuspid valve repair. J Am Coll Cardiol Intv. 2020;Epub ahead of print.
Disclosures
- Taramasso reports consulting for Abbott Vascular, Boston Scientific, 4TECH, and CoreMedic; and having received speaker honoraria from Edwards Lifesciences.
- Fender and Zack report no relevant conflicts of interest.


Comments