Underappreciated by Clinicians, Critical Limb Ischemia Has Dire Fallout for Patients
Strongly linked to morbidity and mortality, CLI merits greater focus and better understanding, according to physicians who spoke at ISET 2017.
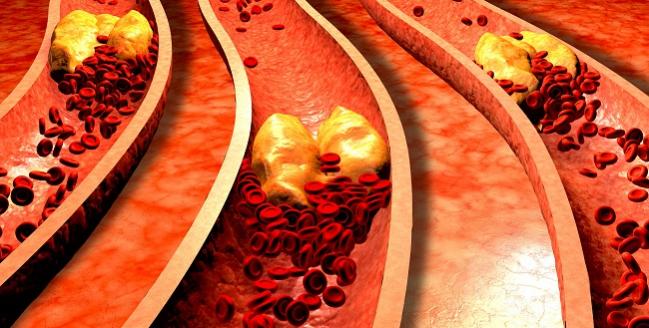
HOLLYWOOD, FL—Critical limb ischemia (CLI), a condition so elusive that it lacks a consistent definition and doesn’t have its own diagnosis code, has a huge impact on patients by way of limb loss and an associated uptick in mortality over follow-up, experts said at a Town Hall devoted to the topic yesterday at the International Symposium on Endovascular Therapy (ISET).
Kicking off the session, Michael Jaff, DO (Newton-Wellesley Hospital, Boston, MA), described CLI patients as “screaming for help.” The first thought of many physicians who see these cases is amputation, but more can be done to curb their morbidity and mortality, he said. “I think our knee-jerk reaction must be, on behalf of our patients, an urgent sense of revascularization, either surgical or catheter-based. [Also] optimal adjuvant medical therapy is critical not only for optimizing outcomes but also for prolonging life.” Wound and infection management are needed, too, he said.
One year after a CLI diagnosis, about a quarter of patients will have died and nearly a third will have had a major amputation, Jaff reported. Quality-of-life measures are on par with those of terminal cancer patients.
William Gray, MD (Main Line Health/Lankenau Heart Institute, Wynnewood, PA), told TCTMD he suspects many cardiologists underappreciate the importance of CLI.
“Something as simple as the cardiologist having the patient take off their shoes when they examine them” could help improve care, given that coronary and peripheral artery disease “share a lot of risk factors and comorbidities,” he suggested. “I don’t think that physicians, when presented with symptoms, are turning away from them by any stretch of the imagination, but I do think that surveillance could be increased a bit, even if it’s just in the early phases of assessment.”
Referring patients with signs of CLI to a specialist is worthwhile, Gray said. “Obviously the most important thing is risk factor modification, because patients don’t die of limb loss, they die of stroke, myocardial infarction, and renal failure.”
Practical Concerns
But physicians and hospitals face many obstacles in addressing CLI, presenters said.
Inconsistencies in how CLI is measured—by varying cutoffs of ankle-brachial index and Rutherford class, which is based on ankle and toe pressure—complicates trial design and comparison of results across studies, Jaff explained. “It makes it harder for us to speak the same language when we can’t even agree on what the objective definitions are.”
Do the best you can. Make sure you make the vessel as big as possible. – William Gray.
Gray noted in his talk that “there remains a paucity of randomized, multicenter, blinded study data to support most device use [below the knee].”
Options include percutaneous transluminal angioplasty and atherectomy, the only on-label therapies for CLI in the United States, as well as BMS, DES, bioresorbable scaffolds, and drug-coated balloons. Right now, the choice among tools should be done on a case-by-case basis, with the goal being acute procedural success and optimization of outcomes, Gray said. “That’s a long-winded way of saying it’s dealer’s choice. Do the best you can. Make sure you make the vessel as big as possible.”
Barry Katzen, MD (Miami Cardiac and Vascular Institute, FL), and others in the session shared details on what it takes to develop a CLI program. Clinicians spearheading such efforts must consider factors such as goals of care, a definition of CLI, objective clinical criteria, treatment protocols or algorithms, data collection, and long-term follow-up.
A chief concern is cost, which is difficult to pinpoint due to the multidisciplinary nature of treatment and expenses related to postacute care, panelists observed.
“To be able to increase awareness, understand the healthcare economic impact, and improve outcomes, we must have the proper diagnostic codes and DRG related to” treatment of CLI, Katzen said. The CLI Global Society, a not-for-profit group dedicated to improving quality of life by preventing amputations and death due to the condition, may be able “to marshal resources to deal with some of those issues that we can’t do only at a single-hospital or single-entity environment,” he added. Katzen noted that about 1 million Medicare patients per year suffer from CLI, with an estimated annual cost of $3 billion.
The BEST-CLI trial, sponsored by the National Heart, Lung, and Blood Institute, may provide some guidance, pointed out study co-chair Alik Farber, MD (Boston Medical Center, MA). The 160-center trial is looking at outcomes, quality of life, and cost in 2,100 patients who are candidates for both open vascular and endovascular surgery. Enrollment is “difficult” but progressing, he said.
Caitlin E. Cox is Executive Editor of TCTMD and Associate Director, Editorial Content at the Cardiovascular Research Foundation. She produces the…
Read Full BioSources
Farber A. Current challenges in the diagnosis and treatment of CLI. Presented at: ISET 2017. February 6, 2017. Hollywood, FL.
Gray W. Making sense of available technologies. Presented at: ISET 2017. February 6, 2017. Hollywood, FL.
Jaff MR. Understanding the epidemic of CLI and its implications. Presented at: ISET 2017. February 6, 2017. Hollywood, FL.
Katzen B. What is a CLI program? Measures of success or benefit. Presented at: ISET 2017. February 6, 2017. Hollywood, FL.
Disclosures
- Farber reports no relevant conflicts of interest.
- Gray reports holding stock in Biomedia, Conteso Medical, and Silk Road; serving as a consultant to Boston Scientific, Medtronic, Shockwave, WL Gore & Associates, Cook, St. Jude Medical, and Intact Vascular; and having research contracts with Boston Scientific, Intact Vascular, and WL Gore & Associates.
- Jaff reports serving on the advisory boards of the American Orthotics/Prosthetics Association, Micell, Primacea, Valiant, and Volcano/Philips. He has equity or holds shares in Primacea (he is also the founder), Embolitech, PQ Bypass, Janacare, MC10, Northwind Medical, Sano V, and Vascular Therapies. He is a noncompensated advisor to Abbott Vascular, Boston Scientific, Cordis, and Medtronic. He has made presentations on behalf of Medscape.


Comments