Using Coronary CTA to Evaluate Suspected CAD May Improve Patient Outcomes
Costs were higher but the risk of MI was lower in patients evaluated with coronary CTA as opposed to functional testing.
Stable patients with suspected CAD may be better off receiving an initial evaluation with coronary CT angiography (CTA) rather than stress testing, despite higher costs, a large, observational study suggests.
The risk of MI was lower through a median follow-up of 3.6 years after coronary CTA (0.8% vs 1.5%; HR 0.71; 95% CI 0.61-0.82), Mads Jørgensen, MB (University of Copenhagen, Denmark), and colleagues report in a study published in the April 11, 2017, issue of the Journal of the American College of Cardiology. Mortality did not differ based on the choice of initial noninvasive testing.
Although coronary CTA also was associated with greater use of invasive cardiac procedures, Jørgensen told TCTMD that he believes the advantage for coronary CTA in terms of MI risk likely stems from changes in medical management that occurred after the evaluation. In particular, patients were more likely to initiate statins and aspirin following a CT scan.
“But it remains very difficult to say what aspects of patient management actually contribute to better prognosis in the long run,” Jørgensen said.
This observational analysis is largely consistent with prior randomized trials comparing functional and anatomical testing, including PROMISE and SCOT-HEART. MI risks were not significantly lower with coronary CTA in those two trials, but there were trends in that direction. Jørgensen et al point out that their study, though limited by the nonrandomized design and lack of some important clinical information, included a much larger patient population followed for a longer period of time; this resulted in a higher number of events.
“The findings from our study really complement the findings from the randomized trials, and I think combining the two study designs gives a much more detailed picture of the whole issue at hand here,” Jørgensen said.
Commenting for TCTMD, James Min, MD (Weill Cornell Medicine/NewYork-Presbyterian, New York, NY), said the findings from this analysis—the largest to explore the issue to date—have mostly been demonstrated before in smaller studies, adding that he thinks the lower risk of MI after evaluation with coronary CTA—which he agrees is likely related to enhanced medical therapy—is “a distinct advantage” for the approach.
When asked why coronary CTA isn’t the go-to approach for evaluating suspected CAD, Min said that it probably is at certain sites. He added, however, that uptake may be slowed by the comfort of physicians with other types of noninvasive testing and by the time it has taken to provide evidence supporting CT.
“It’s taken a while to generate all of the randomized trials, but I think the overwhelming amount of evidence suggests that the use of CT as a first-line noninvasive test seems to be reasonable and, based upon these findings, may actually be superior,” Min said.
Impact of Test Choice on Outcomes Remains Unclear
The optimal noninvasive test for the initial evaluation of symptomatic patients with a low-to-intermediate probability of CAD is not clear, with the choice of either functional or anatomical testing often relying on physician preference and available resources, Jørgensen et al say.
Prior studies have explored differences in diagnostic certainty and short-term surrogate endpoints between testing strategies. Jørgensen said it’s clear using coronary CTA changes patient management, but that the effect on hard clinical outcomes is not certain. The overall results of PROMISE and SCOT-HEART indicated little or no difference in outcomes when coronary CTA was used in place of functional testing, but those trials were limited by low event rates, Jørgensen et al note.
To explore a potential impact on clinical outcomes in a larger cohort, the investigators evaluated Danish nationwide registry data on 86,705 outpatients with suspected stable CAD undergoing an initial evaluation with coronary CTA (38%) or exercise electrocardiography or nuclear stress testing (62%) between 2009 and 2015.
Medication changes, including both initiation and discontinuation, differed between the two groups. Of note, coronary CTA was associated with higher rates of initiation of statins (15.9% vs 9.1%) and aspirin (12.7% vs 8.5%; P < 0.001 for both). Similar changes were seen in the SCOT-HEART trial, in which abnormal coronary CTA results were tied to initiation of antiplatelets, statins, and antianginals and normal results were associated with discontinuation of those drugs, Jørgensen et al point out.
In this study, patients who were evaluated with coronary CTA had higher rates of invasive coronary angiography and exercise electrocardiography and were more likely to undergo revascularization with PCI (3.8% vs 2.2%) or CABG (1.3% vs 1.0%; P < 0.001 for all). Those who initially underwent a functional evaluation, on the other hand, were more likely to undergo subsequent testing with nuclear stress imaging and coronary CTA.
Jørgensen noted that among the patients referred for catheterization after the initial test, revascularization was more often performed in the coronary CTA group, which could indicate that the greater use of invasive management was appropriate.
Cost Issues
In line with prior studies, costs related to subsequent testing, invasive procedures, and medications in the first 120 days were higher following coronary CTA. Nonetheless, Jørgensen said the absolute difference in total cost between the two strategies—$1,408 versus $1,006 in US dollars (P < 0.001)—was not that great.
“The question remains whether the higher costs of using coronary CTA as an initial test are justified by improved clinical outcomes,” he and his colleagues write in their paper, noting that the reduced risk of MI may justify the added expense. “We have not, however, performed a formal cost-effectiveness evaluation of coronary CTA versus functional testing, which would require additional data on late costs and quality of life, and a formal model of the effects on long-term outcomes.”
Min said that the cost associated with coronary CTA is a legitimate issue that needs to be studied, but he emphasized the benefit of reducing MIs.
“[Cost is] an issue that needs to be evaluated further,” he said. But, he added, “For me, as a clinician, I care about clinical outcomes first and then we’ll figure out the cost later. Saving MIs I think should be our primary concern.”
In an accompanying editorial, Ron Blankstein, MD (Brigham and Women’s Hospital, Boston, MA), and colleagues highlight the importance of cost containment in the current environment.
“The identification of patients who do not require any further testing, or those who may be evaluated with a less expensive exercise treadmill test alone, could be used to offset the higher costs of CTA noted [in the study],” they write. “The most appropriate way to deal with the incorporation of a new technology that seems to be beneficial, yet costly, is to establish criteria on how to select optimally between the available testing options, rather than assume (as clinical trials sometimes do) that one test is superior across all scenarios.”
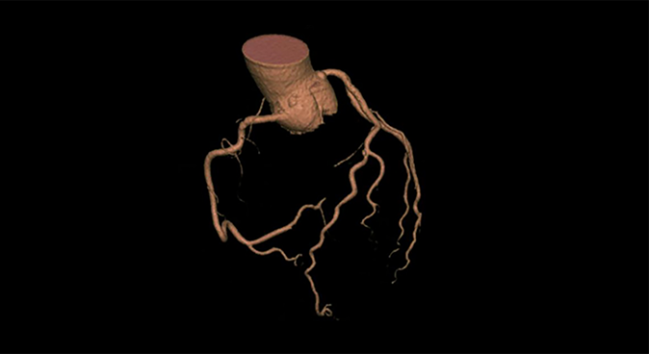
Photo Credit: Society of Cardiovascular Computed Tomography
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Jørgensen ME, Andersson C, Nørgaard BL, et al. Functional testing or coronary computed tomography angiography in patients with stable coronary artery disease. J Am Coll Cardiol. 2017;69:1761-1770.
Blankstein R, Bittencourt MS, Bhatt DL. Coronary CTA in the evaluation of stable chest pain: clear benefits, but not for all. J Am Coll Cardiol. 2017;69:1771-1773.
Disclosures
- The study was supported by a grant from the Lundbeck Foundation to the Innovation Center Denmark to fund the Lundbeck Foundation Clinical Research Fellowship for Jørgensen at Stanford University’s Department of Health Research and Policy.
- Jørgensen reports receiving additional financial support from the Snedkermester Sophus Jacobsen and hustru Astrid Jacobsens Foundation.
- Blankstein reports serving as a member of the advisory board for Amgen and as a member of the board of directors for the American Society of Nuclear Cardiology and the Society of Cardiovascular Computed Tomography.
- Min reports receiving grant funding from GE Healthcare, serving as a consultant to Heartflow, and serving on the medical advisory board of Arineta.


Comments