VT, No Matter Its Source, Benefits From Early Catheter Ablation: PAUSE-SCD
Unlike earlier trials, this one included nonischemic and arrhythmogenic RV cardiomyopathy, with a special focus on Asia.
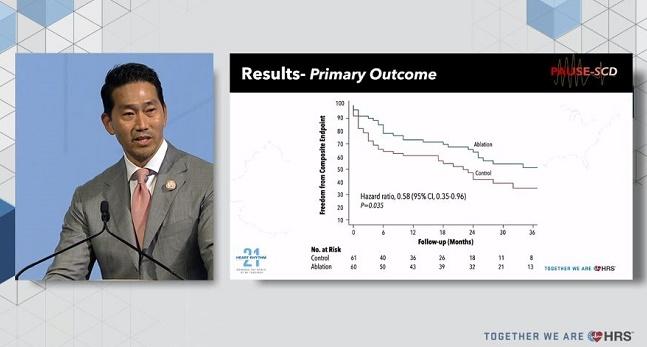
Compared with patients given only conventional medical therapy along with their ICD, researchers saw a significant 42% drop in the combined risk of VT recurrence, CV hospitalization, or death among those who received ablation, Roderick Tung, MD (University of Chicago, IL), told virtual and live attendees of the Heart Rhythm Society 2021 Scientific Sessions.
He stressed that PAUSE-SCD is unique in that it enrolled a mix of monomorphic VT patients—not only those with ischemic cardiomyopathy but also those with nonischemic and arrhythmogenic right ventricular cardiomyopathy (ARVC). Overall, “there is a paucity of multicenter randomized trials to assess the role of early first-line catheter ablation for [monomorphic] VT,” he said. “As a matter of fact, the three that have shown benefit”—SMASH-VT, VTACH, and VANISH—“have exclusively enrolled ischemic cardiomyopathy patients.”
Another point of interest is that the trial enrolled patients in Asia, “our largest populous continent on the globe at risk for sudden cardiac death,” Tung added.
Speaking with the media at HRS, Tung highlighted the timing of ablation in PAUSE-SCD. That it occurred days ahead of ICD implantation “is a total paradigm shift and departure from standard clinical medicine,” he said.
“Typically the defibrillator is put in and we look to see if there are consequences, and then we think about ablation as a palliative, last-resort strategy,” Tung explained, adding that if their results bear out, ablation “really needs to be introduced in the dialogue between [physicians] and patients at risk for sudden cardiac death at the time of ICD implantation.”
China, Japan, Korea, and Taiwan
The investigator-initiated trial enrolled patients with structural heart disease, ejection fraction < 50%, and monomorphic VT who had an indication for ICD at 11 sites in China, Japan, Korea, and Taiwan. The 133 participants who consented to receiving an ICD were randomized to either catheter ablation (done within 90 days of ICD implantation) or conventional medical therapy, while another 47 who declined these options were included in an ablation-only registry without ICD. Antiarrhythmic drugs and choice of epicardial approach were at the discretion of the treating physician and local practice.
Among the 121 randomized patients included in the main intention-to-treat analysis, the median age was 55 and median ejection fraction was 40%. Around one-third each had ischemic, nonischemic, and ARVC. Nearly half presented with tolerated VT (46%) and half with syncope or near syncope (47%), while 5% were in cardiac arrest; the others had primary prevention indications. Amiodarone was given to 35%, with no imbalance between the study arms. Ablation was done at a median of 2 days before ICD implantation.
The registry patients, by contrast, tended to be younger (median age 46 years) and to have higher ejection fraction (median 60%). They were much more likely than the randomized cohort to have ARVC (70.2%) and less likely to have ischemic cardiomyopathy (8.5%).
With ablation, 80% of cases achieved noninducibility. Median times for radiofrequency and procedure duration were 45 minutes and 240 minutes, respectively.
At a median follow-up of 36 months, the RCT’s primary endpoint of freedom from VT recurrence, CV hospitalization, or death was less common for controls versus the ablation-treated patients (HR 0.58; 95% CI 0.35-0.96; P= 0.035).
“These results diverged early, and the curves remained separate to 3 years and the completion of the study,” Tung reported. This was largely driven by freedom from VT recurrence (HR 0.51; 95% CI 0.29-0.90; P = 0.021). Outcomes were generally similar across subgroups—including by etiology—but men and patients without atrial fibrillation appeared to fare better with ablation, Tung said, noting that the numbers were too small to draw conclusions. There also were positive but nonsignificant trends favoring patients with ARVC and ejection fractions > 30%.
Additionally, “when examining that registry group, we observed that the ablation sans ICD had comparable outcomes to those randomized to ablation with ICD,” Tung said. Patients randomized to ICD alone, on the other hand, had more primary-endpoint events than did the registry patients who received ablation alone (HR 1.88; 95% CI 1.08-3.29; P= 0.019).
In the RCT, there were five complications related to ablation, for a rate of 8%: type B aortic dissection, aortic valve cusp prolapse (retrograde), LV perforation during endo ablation, delayed effusion 47 days after ablation, and RV puncture during epicardial access without sequelae. Five deaths occurred in the ablation group (one each due to VT, heart failure, and cerebrovascular accident 6 months after ablation, plus two lung cancers) and four in the control group (two due to heart failure, one to pulmonary nodular amyloidosis 4 days after LV assist device implantation, and one unknown).
In the ablation registry, there was one LV inferolateral wall perforation and three deaths (due to multiorgan dysfunction 4 days after ablation, stomach cancer, and sudden death).
Paul A. Friedman, MD (Mayo Clinic, Rochester, MN), in discussion following the presentation, pointed out that monomorphic VT represents a “vast minority” of patients who receive ICDs, as opposed to the majority who get an ICD as primary prevention. “So it is a smaller cohort, I think, as we put it into context,” he said.
Another question is why data from three prior RCTs haven’t yet changed standard practice, said Friedman, suggesting that it may come down to concern about the potential for significant complications with ablation. “When we weigh the calculus as we’re approaching the patient with monomorphic ventricular tachycardia, we have to decide [if the benefit is worth the risk]. So I think that it is a difficult decision to make, to prophylactically ablate someone, candidly speaking in the real world,” he commented.
More interesting to Friedman were the registry patients who did so well despite not receiving an ICD.
To TCTMD, Tung reiterated that PAUSE-SCD draws attention to the “global health crisis of sudden cardiac death” by focusing on Asia, where many people may be unable to afford an ICD and the devices aren’t covered by insurance. Moreover, he raised the possibility that ICDs may not be the best choice for patients with nonischemic cardiomyopathy, suggesting that a “future trial to look at ablation without background ICD therapy may be justifiable.”
Caitlin E. Cox is Executive Editor of TCTMD and Associate Director, Editorial Content at the Cardiovascular Research Foundation. She produces the…
Read Full BioSources
Tung R. A randomized trial of early first-line catheter ablation for ventricular tachycardia: results from the Pan-Asia United States Prevention of Sudden Cardiac Death Trial (PAUSE-SCD). Presented at: HRS 2021. July 29, 2021.
Disclosures
- Tung reports receiving speaking fees and serving on the advisory boards of Abbott, Biotronik, Boston Scientific, and Medtronic, as well as receiving research grant support from Abbott.




Comments