Will Percutaneous Mitral Repair Catch Up or Surpass Surgery? Experts Make Their Predictions
As COAPT and MITRA-FR crest the horizon, surgeons and cardiologists alike have plenty of opinions about the future of repair in severe MR.
CHICAGO, IL—Eagerly awaited results from two percutaneous mitral valve edge-to-edge repair trials are finally cresting the horizon. It’s confirmed: MITRA-FR will be released at the 2018 European Society of Cardiology (ESC) Congress in Munich, Germany, while COAPT will come out 1 month later at TCT 2018.
Many of the people who have been active in the MitraClip (Abbott) field since its infancy are now offering some tentative bets as to how the trials may shake out and, taking the longer view, asking just how edge-to-edge therapies alone or in tandem with other percutaneous procedures will stack up against surgical repair for mitral regurgitation (MR). Questions dogging this field include the lack of comparably designed studies in the surgical field, uncertainty as to which patients should be treated and when, and the long-term clinical relevance of residual MR—a relatively common finding among patients treated with percutaneous approaches.
Ted Feldman, MD (Evanston Hospital, Chicago, IL), led the earliest studies of the MitraClip and was the first to implant the device in the United States back in 2003. He took to the stage here at the 2018 Structural Heart Disease Summit to make the case that percutaneous annuloplasty rings, coaptation clips, and chordal replacement devices will ultimately match or exceed the benchmark set by surgery. In the case of the MitraClip, Feldman continued, its superior safety gives it the edge over surgery while the residual MR, a key predictor of worse outcomes in the surgical literature, has not emerged as an important precursor for reintervention or mortality out to 5 years among MitraClip-treated patients.
Moreover, acute success has also improved radically since the EVEREST I trial, with percent success rising from the low 60s to nearly 100% in the GRASP-IT trial.
Offering a quick overview of the other annuloplasty and chordal devices now in early trials, Feldman made the point that, by contrast, the surgical evidence base does not have the backing of rigorous clinical studies, but rather is “eminence-based,” supported by a healthy dose of bravado. In the percutaneous space, he added, “our ability to approximate the surgical toolbox is rapidly evolving.”
Variety Matters
Not so fast, said Gilbert Tang, MD (Mount Sinai Health System/Icahn School of Medicine, New York, NY), who took the stage after Feldman. Or at least, “not yet.”
Percutaneous procedures, at least for now, do not offer the variety of approaches that surgery can offer, he argued, pointing out that MR comes in myriad forms. Different MR etiology, mitral lesions, and patient risk profile all play an important role. And while transcatheter therapies have evolved to approximate edge-to-edge, annuloplasty, and chordal replacement procedures, no percutaneous therapy is able to perform resection and reconstruction, a common surgical technique, Tang said.
The presence of concomitant diseases such as atrial fibrillation, tricuspid disease, and coronary artery disease should also tip a heart team in favor of a surgical approach, he said.
Perhaps most importantly, moderate or greater MR has been documented in the range of 21% to 41% in MitraClip studies, while chordal and annuloplasty devices in the small series to date, are associated with postprocedure MR rates ranging from 10% to 32%.
Last but not least, “each device performs only one function,” Tang concluded, with limited or no ability to treat complex pathologies or to repair endocarditis, leaflet perforation, and type III dysfunction. “Procedure times are also long,” he said, “particularly for combination therapies.”
‘In Some Way Better?’
In discussion following the debate, session co-moderator Gregg Stone, MD (NewYork-Presbyterian/Columbia University Irving Medical Center, New York, NY), co-PI for COAPT, posed a provocative question: “Is it possible . . . that transcatheter approaches are in some way better than surgical approaches, or is edge-to-edge different somehow with MitraClip than with the Alfieri [surgical stich procedure]? Or was there just not enough data with Alfieri?”
Panelist Francesco Maisano, MD (Klinik für Herz- und Gefäßchirurgie, Universitätsspital Zürich, Switzerland), who fielded the question, suggested that “all of the above” may be true. The fact that percutaneous procedures can be done on a beating heart, allowing operators to assess their handiwork in real time, may be a key reason for success, Maisano offered. “There is obviously a signal that, using transcatheter techniques, you can at least reproduce what surgery does.”
Karl-Heinz Kuck, MD (Asklepios Klinik St. Georg, Hamburg, Germany), pointed to the fact that transcatheter mitral innovation has progressed at a galloping pace not matched by the surgical field and these advances may propel percutaneous therapies into the lead.
“We are just in the middle of the development, we are not at the end, so I’m 100% convinced that things are getting better and better and that we need to rechallenge surgery every day,” Kuck said. “I’m extremely optimistic that we can improve this.”
Kuck also observed that the evidence presented by Feldman and Tang was based on first- and second-generation MitraClip devices, used by physicians still becoming proficient with the procedure. Citing early results with the latest-generation MitraClip, the XTR, presented yesterday, Kuck said: “It’s clear that the XTR cannot be compared with the original device.”
But going forward, is it acceptable to have residual MR following one procedure with a plan to tackle any residual leakage with a second procedure a few months later? That was the question posed by session co-moderator Jason Rogers, MD (University of California, Davis).
In response, cardiothoracic surgeon Steven Bolling, MD (University of Michigan, Ann Arbor), reminded the audience that “the vast majority of the data show that recurring or residual MR makes for a bad outcome long-term, so that’s why we aim for an MR of zero at the time we operate, and that predicts the best outcome. I would say that the biology of mitral regurgitation will not change with the method of delivery.”
As to whether getting to zero regurgitation with a staged procedure can achieve the same outcomes, he said, “I think that is probably an okay strategy, but I think to leave the patient with any regurgitation long-term will be a bad answer for that patient.”
Looking Ahead to the Trials
Answers from COAPT and MITRA-FR will set the stage for some of these new questions to be broached or for old questions to be asked anew. Maisano repeated a prediction he’s made in the past, namely that COAPT will be negative because it enrolled patients too late in their disease course. The trial enrolled patients who had had at least one hospitalization for heart failure in the past year and to have had treatment optimized for their heart failure, coronary disease, and heart rhythm abnormalities, cardiac resynchronization therapy (CRT), if needed.
“This is a trial that has been done testing what happens if you open a parachute too late,” he said. He’s already looking ahead to subsequent studies which would take a “synergistic approach” by treating patients earlier in the course of their heart failure with optimal medical therapy, CRT if needed, and MitraClip before LV dysfunction has progressed too far.
Taking the opposite view, Scott Lim, MD (University of Virginia, Charlottesville), drew heavily on Maisano’s own publications to underscore the point that the MitraClip’s safety is now indisputable, while also reducing patients’ symptoms and improving their exercise times.
“Based on this [observational] data, golly!” Lim quipped. “I think we have to look at the randomized clinical trials and say they are likely to be positive.”
Rogers, however, pointed out that the screening process for COAPT was so strict that only a minority of patients made it into the trial and these are not representative of the vast majority of patients in whom the MitraClip might help. “The patients that are referred to us are symptomatic, they’re been hospitalized, they’re having diuretic dose adjustments, and the referring physician is calling us and saying: please do something. In general, these were not the patients who were enrolled in COAPT,” he commented.
As such, it might just be that patients enrolled in these two eagerly awaited trials “just weren’t sick enough to demonstrate a treatment effect,” Rogers hinted.
In response, Lim pointed out that total mortality numbers from MITRA-FR were already released and point to a higher than expected mortality among patients in both treatment arms. COAPT, meanwhile, was expanded to include more patients, in part because too many of those enrolled were dying, thereby limiting the study’s ability to look at heart failure readmissions.
“So this is still a very sick population,” Lim said.
Maisano had one other prediction, pointing out that the two trials used different definitions of severe MR, which will further complicate efforts to understand their results side-by-side. “There are substantial differences in the two trials, and I would not be surprised to see different results from the two trials,” he stressed.
Feldman, who spoke with TCTMD for an upcoming episode of On Record, hedged his bets. “TAVR sort of created an unrealistic expectation that we can have valve trials that are unequivocal,” he said. “That’s a once-in-several-lifetimes experience. There are many, many things that we could see [from COAPT] that could give us positive signals without actually hitting absolutely positive primary endpoints, and if I have to make a prediction, that would be it, that we will get some signals . . . on quality of life, for example.”
He also offered the possibility that patients with or without CRT might also yield different results, but added, “Maybe we’ll be surprised.”
Only time will tell. MITRA-FR is slated for presentation during the August 27 Hot Line session at ESC 2018, while COAPT will be one of the late-breakers during the TCT 2018 meeting held September 21-25 in San Diego, CA.
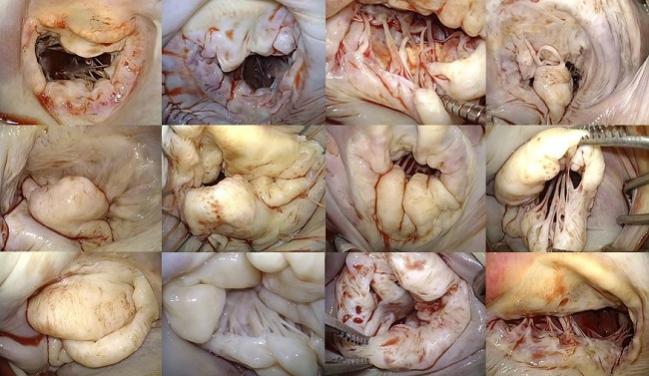
Photo Credit: Tang GHL. Can Transcatheter Mitral Rings, Edge-to-Edge, and Chords Match or Exceed Open Surgical Procedures? NO! The Structural Heart Disease Summit. Presented at: Structural Heart Disease Summit. June 22, 2018. Chicago, IL.
Shelley Wood was the Editor-in-Chief of TCTMD and the Editorial Director at the Cardiovascular Research Foundation (CRF) from October 2015…
Read Full BioSources
Multiple presentations. Transcatheter Mitral Challenges and Controversies. Structural Heart Disease Summit. June 22, 2018. Chicago, IL.
Disclosures
- Feldman reports receiving grant support from Corvia, as well as grant support from and consulting for Abbott, Boston Scientific, Edwards, and WL Gore. He also reports stock options with Mitralign and Cardiac Dimensions.
- Tang reports being a faculty trainer and consultant for Abbott Vascular and serving as a consultant to Neochord.
- Maisano reports consulting for Abbott, Valtech Cardio, Medtronic, Edwards Lifesciences, and St Jude, and receiving research grants from Abbott, ValtechCardio, Medtronic, Edwards Lifesciences, St Jude, and Biotronik. He is also the founder of 4Tech, TSP Medical, and Affix and receives royalties from Edwards Lifesciences.
- Stone reports equity in Ancora, serving as a consultant for Valfix and Gore, and being an uncompensated PI for Abbott.


Comments