Window for IV Thrombolysis in Stroke May Stay Open Twice as Long With Imaging Selection
The prematurely halted EXTEND trial suggests benefits can be seen in patients who present within 9 hours or who wake up with a stroke.

HONOLULU, HI—Patients with acute ischemic stroke who have salvageable brain tissue identified with advanced imaging appear to benefit from IV tissue plasminogen activator (tPA) beyond guideline-recommended time windows, results of the EXTEND trial show.
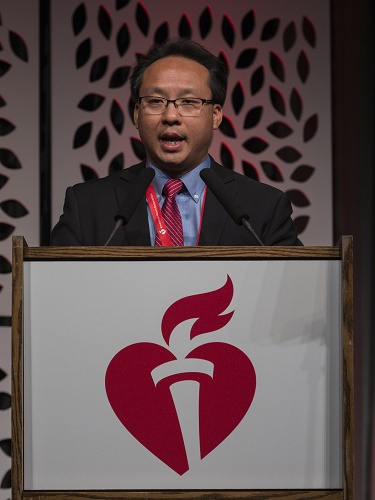
Patients presenting between 4.5 and 9 hours after symptom onset or with a wake-up stroke were more likely to achieve an excellent functional outcome at 90 days if they were treated with IV thrombolysis instead of placebo (35% vs 29%; adjusted relative risk 1.44; 95% CI 1.01-2.06), Henry Ma, PhD (Monash University, Melbourne, Australia), reported last week at the International Stroke Conference.
The findings were similar in a per protocol analysis, which also showed that several secondary outcomes favored use of tPA.
“EXTEND is the first positive thrombolysis trial in an extended time window using automated penumbral imaging,” Ma said during his presentation.
Though a lot of excitement in the world of acute stroke interventions over the past 4 years has been driven by positive trials of mechanical thrombectomy—with evidence now supporting its use up to 24 hours after symptom onset in select patients—IV thrombolysis continues to be a mainstay of treatment. Guidelines, in fact, contain strong recommendations to use tPA as quickly as possible in eligible patients, with the window extending out to 4.5 hours of stroke onset or the time the patient was last known well. It is recommended that eligible patients receive IV thrombolysis even if endovascular therapy is being considered.
Ma said there is evidence from imaging studies suggesting that an ischemic penumbra—ischemic but still viable brain tissue—can exist for up to 24 hours and that restoring blood flow to that area can improve clinical outcomes. He pointed out that the phase II EPITHET trial, which used MRI perfusion imaging to identify patients with a clinically significant penumbra, indicated that IV thrombolysis could be effective beyond the 4.5-hour time window.
EXTEND Trial
The phase III EXTEND trial—conducted at 22 centers in Australia, 11 in Taiwan, and one each in New Zealand and Finland—was designed to explore that concept further. The trial included patients with acute ischemic stroke and a significant penumbral mismatch who either presented within 4.5 to 9 hours after stroke onset (about one-third) or woke up with a stroke (about two-thirds). Imaging was done with CT perfusion or MR diffusion/perfusion with RAPID automated software (iSchemaView).
The initial intent was to enroll 310 patients, but recruitment was stopped after publication of the WAKE-UP trial, which showed that patients with acute stroke and an unknown time of onset derived a benefit from imaging-guided IV thrombolysis. Ultimately, EXTEND included 225 patients.
The primary endpoint was excellent functional outcome—defined as a modified Rankin Scale (mRS) score of 0 to 1—at 90 days. Ma showed that this was improved with tPA in the intention-to-treat analysis before focusing on the per protocol analysis, which excluded 14 patients from the thrombolysis group and seven from the placebo group and was therefore underpowered.
The median time from last known well to therapy was about 10 hours in the tPA arm and 9 in the placebo arm. Overall, roughly 70% of patients had large-vessel occlusions, “which could be amenable to thrombectomy,” Ma said, noting, however, that no patients in the trial underwent endovascular therapy.
In the per protocol cohort, thrombolysis increased the rate of excellent functional outcome at 90 days (37% vs 29%; adjusted RR 1.45; 95% CI 1.01-2.10). Among secondary endpoints, tPA came out on top for mRS scores of 0 to 2 at 90 days (51% vs 43%) and the following outcomes at 24 hours: early neurological improvement (25% vs 10%), achievement of 90% reperfusion (51% vs 28%), achievement of 50% reperfusion (73% vs 53%), and complete recanalization (70% vs 40%; P < 0.05 for all).
By 90 days, 11.1% of patients who received tPA had died, compared with 9.5% who received placebo (P = 0.77). The rate of symptomatic intracranial hemorrhage at 36 hours was higher in the thrombolysis arm (6% vs 1%; P = 0.066).
Ma said the increase in hemorrhage has also been seen in other trials of IV thrombolysis, “but this was not associated with increased mortality and did not negate the positive result of improved rate of excellent functional outcome.”
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Ma H. Extending the time for thrombolysis in emergency neurological deficits (EXTEND). Presented at: ISC 2019. February 8, 2019. Honolulu, HI.
Disclosures
- Study drug was supplied by Boehringer Ingelheim. iSchemaView provided the RAPID software platform.
- Ma reports no relevant conflicts of interest.


Comments