AMBULATE: Venous Closure Device Pays Off After Catheter Ablation
Among other benefits, the VASCADE MVP system shortened time to ambulation and boosted patient satisfaction.
For patients who require multisite venous access for catheter ablation procedures, the VASCADE MVP venous vascular closure system (Cardiva Medical) provides a variety of benefits, including a shorter time to ambulation and increased patient satisfaction, results of the randomized AMBULATE trial show.
Average time to ambulation—the primary endpoint—was 2.8 hours when the device was used and 6.1 hours when manual compression was used (P < 0.0001), according to researchers led by Andrea Natale, MD (Texas Cardiac Arrhythmia Institute, Austin).
The study, initially presented last year at the American Heart Association 2018 Scientific Sessions in Chicago, IL, also showed that use of the device positively impacts multiple secondary endpoints, reduces use of opioids, and improves patient satisfaction regarding the duration and comfort of bedrest and associated pain.
“This is one of the first randomized trials that really looks at workflow, and it shows that the patient experience is dramatically improved when you can shorten these times,” senior author Mintu Turakhia, MD (Stanford University and VA Palo Alto Health Care System, CA), told TCTMD.
“It’s important for people to recognize that getting people up and out of bed and possibly home is important and feasible and achievable,” he continued. “We’ve seen these strides in traditional surgery, we’ve seen it in [cardiac] cath, and I think now it’s moved into EP [electrophysiology]. This trial supports the use of this device to do that, and I think we make a strong case here for it. But no matter how it’s done, really the field should think hard about how to shorten that postprocedure experience.”
Commenting for TCTMD, Jonathan Hsu, MD (UC San Diego Health, La Jolla, CA), said, “Vascular closure, particularly in atrial fibrillation ablation, is important to think about for electrophysiologists due to the fact that the field is moving towards anticoagulation before, during, and after the procedure.”
He said it’s worth exploring whether devices like this one will have benefits for patients—in terms of both clinical outcomes and quality of life—and for workflow in electrophysiology labs. “These are all important issues to consider when we’re talking about an additional device for their procedure,” Hsu advised. “As long as the vascular closure is safe and effective, I think we certainly need to consider it in our daily practice.”
The AMBULATE findings were published online October 29, 2019, ahead of print in JACC: Clinical Electrophysiology.
AMBULATE Trial
Turakhia noted that for A-fib ablations in particular, procedural volume has continued to rise along with the maturity of the technology. Procedure times are shorter, there are better tools to isolate the pulmonary veins, mapping systems have improved, and there is better knowledge about how to achieve a durable result, he said. Preprocedural preparation has become easier as well, because typically anticoagulation is not discontinued.
But those advancements in pre- and intraprocedural aspects of ablation have not occurred in the postprocedural setting, where most patients still require prolonged bedrest that can last up to 8 hours to ensure hemostasis. How to speed up the postprocedure workflow, and at the same time improve patient outcomes, remains an unmet need, Turakhia said.
He pointed to the field of interventional cardiology and efforts to increase same-day PCI as an example. “We in EP I think have been a little bit behind in our ability to make the postop experience more efficient.”
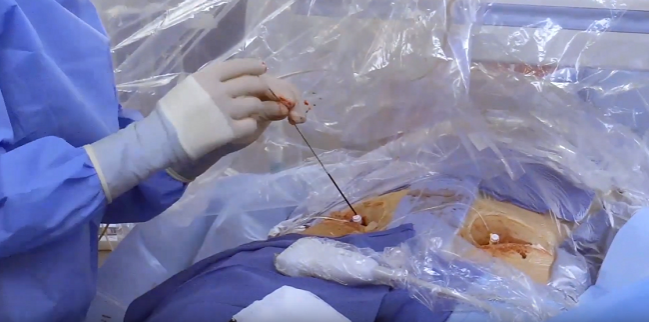
Venous closure devices may provide a solution. The VASCADE MVP system, which received US Food and Drug Administration approval in December 2018 and recently received CE Mark approval in Europe based on the AMBULATE results, is designed to establish hemostasis in patients who require multiple venous access sites for catheter-based EP procedures employing 6- to 12-Fr diameter sheaths, such as A-fib ablation and left atrial appendage occlusion. Closure involves placement of a collagen plug, which will eventually absorb into the body, to stop the bleeding.
The AMBULATE trial, conducted at 13 centers, pitted the device against manual compression in 204 patients who underwent catheter ablation (mostly for A-fib) requiring three or four access sites in the femoral veins. Most patients (84%) were on some type of anticoagulation before the procedure, and both periprocedural anticoagulation management and use of protamine reversal were left to the discretion of the operator.
Aside from reducing the time to ambulation compared with manual compression, use of the closure device shortened mean values for:
- Time to hemostasis (6.1 vs 13.7 minutes; P < 0.0001)
- Time to closure eligibility (10.5 vs 37.6 minutes; P < 0.0001)
- Total postprocedure time (3.1 vs 6.8 hours; P < 0.0001)
- Time to discharge eligibility (3.1 vs 6.5 hours; P < 0.0001)
The vast majority of access sites closed with the device (90%) reached hemostasis within 7 minutes. In contrast, 90% of sites closed with manual compression required 20 to 25 minutes to achieve hemostasis.
With the advent of newer devices, and devices mainly specialized for venous closure that may have a higher rate of actual venous closure, I think that it’s certainly worth revisiting this . . . Jonathan Hsu
Although time to discharge eligibility was reduced with the device, average time to actual discharge was the same in both arms of the trial (21.8 hours). Most patients stayed overnight, which “may reflect longstanding institutional practice,” the authors note. “We are cautiously optimistic that shortened time to ambulation may in turn facilitate shorter time to discharge, including obviating the need for an overnight stay in some cases.”
Use of the VASCADE MVP system was safe, with no major access-site complications reported within 30 days. There were two minor access-site complications—one infection and one pseudoaneurysm—in the device group and five in the manual-compression group (P = 0.45). There were no deaths in the trial.
Surveys indicated that patient satisfaction was higher when the closure device was used, with significantly improved assessments of the duration and comfort of bedrest and of pain associated with bedrest. Those differences in satisfaction were amplified among patients who had undergone a prior ablation.
Focus on Patient Experience
Hsu said cost would be an issue when considering use of a closure system like VASCADE MVP—and Turakhia said an economic analysis is planned—but added that it would be difficult to downplay the positive impact of shorter bedrest and other effects on the patient experience.
One of the biggest issues for patients undergoing ablations is the need to remain supine for several hours after the procedure, leading to musculoskeletal pain from the bedrest itself in many cases, Hsu said.
“If this device can help with assuring vascular closure and allowing the patient to ambulate and not have musculoskeletal pain and therefore not need additional medications, that’s beneficial both for the patient and the physician/hospital,” he said.
Hsu said that in his center, the standard method for establishing hemostasis has shifted from manual compression to use of closure devices and then—after some failures—back to manual compression.
“With the advent of newer devices, and devices mainly specialized for venous closure that may have a higher rate of actual venous closure, I think that it’s certainly worth revisiting this aspect as the field moves towards more perioperative anticoagulation,” he said, adding that AMBULATE “is an important study that needs to be considered in practice across the United States.”
Turakhia said “all of us in the field really should be thinking about how to make A-fib ablation in the average patient a same-day discharge procedure . . . and that’s very important as we do more of these but also I think for each and every patient they’ll be much happier when they go home.”
Photo Credit: Adapted from Cardiva Medical video.
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Natale A, Mohanty S, Liu PY, et al. Venous vascular closure system versus manual compression following multiple-access electrophysiology procedures: results from the multicenter randomized AMBULATE trial. J Am Coll Cardiol EP. 2019;Epub ahead of print.
Disclosures
- The study was sponsored by Cardiva Medical.
- Natale reports receiving compensation for services from Boston Scientific, Abbott, and Medtronic and serving on the speakers’ bureau for Biosense Webster, Biotronik, and Baylis Medical.
- Turakhia reports receiving compensation for services from Abbott, Precision Health Economics, Cardiva Medical, iRhythm Technologies, iBeat, Novartis, Biotronik, Sanofi-Aventis, Pfizer, and Medtronic; serving on the speakers’ bureau for Medscape; hold equity interests/stock options in AliveCor, Zipline Medical, iBeat, and E-Safe; and receiving research grants from Cardiva Medical, AstraZeneca, Janssen, Medtronic, the Veterans Administration, Boehringer-Ingelheim, Apple, the American Heart Association, Bristol-Myers Squibb, and SentreHeart.
- Hsu reports receiving honoraria from Medtronic, Boston Scientific, Abbott, Biotronik, Biosense Webster, Janssen Pharmaceuticals, and Bristol-Myers Squibb; receiving research grants from Biosense Webster and Biotronik; and having equity interest in Acutus Medical and Vektor Medical.


Comments