Bicuspid SAVR Outcomes Meet or Beat Tricuspid in STS Database
Surgeons and referring physicians will need to pay careful attention to comorbidities when making decisions on care.
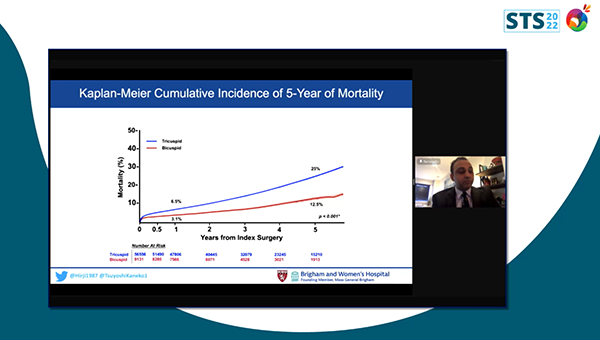
Patients with bicuspid aortic valve stenosis who undergo SAVR do as well as those with tricuspid valves, with a lower rate of risk-adjusted long-term death, according to a new analysis from the Society of Thoracic Surgeons (STS) Adult Cardiac Surgery Database.
A number of recent TAVI trials and registry analyses have compared outcomes in tricuspid and bicuspid aortic valves—a pressing question as the technology moves into younger, lower risk patients. But long-term TAVI data are needed, and multiple questions remain as clinicians and patients weigh their long-term options, with surgery typically considered to be the gold standard in younger adults.
“Surprisingly, there's really no data on the SAVR side looking at the bicuspid patients, and there's a lot of hurdles in doing randomized-controlled studies,” said Tsuyoshi Kaneko, MD (Brigham and Women’s Hospital, Boston, MA), who along with Sameer Hirji, MD (Brigham and Women’s Hospital), analyzed data on 65,687 patients from 1,146 centers in the United States undergoing index isolated SAVR between 2011 and 2018.
“The bottom line is that the SAVR outcomes of these bicuspid patients were excellent,” Kaneko told TCTMD.
Presenting the findings earlier this week at the virtual STS 2022 meeting, Hirji said the data provide key benchmarks on short- and long-term outcomes in bicuspid patients that can aid the heart team in clinical decision-making in the context of lifetime management.
“Bicuspid aortic valves are an important but very misunderstood disease process, both in surgery and the transcatheter space,” said discussant Tom C. Nguyen, MD (University of California San Francisco, CA). He noted that from a surgical standpoint AVR on a bicuspid valve tends to be “trickier” than on a tricuspid valve, raising the question of why 5-year mortality ended up being lower than in the tricuspid group.
Hirji said several variables might account for the difference in mortality, including unmeasured confounding and genetics. According to Kaneko, bicuspid patients are more likely than tricuspid patients to have calcification that is focal to the valve itself and tend to be healthier overall.
Fewer Readmissions in Bicuspid Patients
In the study, 9,131 patients (13.9%) had BAV. Compared with the tricuspid patients, those with BAV were younger, less often female, and had lower STS-PROM scores, and lower risk profiles (ie, diabetes, hypertension, and NYHA class III/IV). BAV patients also were less likely than the tricuspid group to undergo urgent procedures. By STS PROM score, 92% of BAV patients were low risk versus 78.5% of the tricuspid group (P = 0.001).
While a survival benefit was observed across all risk groups, in those with STS PROM score < 3%—which accounted for most of the population—the risk-adjusted 5-year mortality was lower in the bicuspid versus tricuspid group (HR 0.69; 95% CI 0.64-0.76).
In secondary analyses, bicuspid patients had a lower 5-year adjusted risk for heart failure readmission compared with the tricuspid group (HR 0.64; 95% CI 0.56-0.72), as well as reduced risks of readmission for stroke (HR 0.74; 95% CI 0.65-0.85), for bleeding (HR 0.82; 95% CI 0.72-0.93), or for any CV reason (HR 0.88; 95% CI 0.83-0.85).
Commenting on the study for TCTMD, Raj Makkar, MD (Cedars-Sinai, Los Angeles, CA), suggested that comorbidities likely explain some of the higher mortality in the tricuspid patients, “partly because bicuspid patients are developing aortic stenosis at a younger age.” And while more and more patients with bicuspid disease may be sent for TAVI, higher-risk patients with bicuspid AS are typically treated surgically, he added. “A lot of these things are not captured in the STS scores.”
Makkar pointed to the subgroup of patients with ejection fraction less than 50% by way of example. Here, Kaneko and Hirji’s data indicated that SAVR in bicuspid patients with an EF of 50% or greater was associated with a 5-year mortality risk reduction of 31% in relation to tricuspid patients (HR 0.69; 95% CI 0.63-0.75). but no similar, statistically significant risk reduction was evident among those with ejection fraction less than 50%, for whom 5-year mortality was “substantial,” Makkar noted.
In after the Q&A following Kaneko’s presentation, Nguyen wondered if the data could serve as “the final hammer for TAVR, based on recent data that bicuspid patients do worse with TAVR and that you should be doing SAVR instead of TAVR in patients with bicuspid aortic stenosis.”
Kaneko, to TCTMD, said that view is “a little extreme,” adding that “what this paper is really suggesting is that we have to have a very careful, balanced discussion [about] TAVR and SAVR. Everybody wants TAVR. That's the reality, right? Nobody wants open-heart surgery. But if they have a significant calcification throughout the valve, the right thing to do in that patient is to go for surgery and we have the tools to support that.”
Makkar stressed that comparing registry data to draw conclusions on TAVI versus SAVR in bicuspid cohorts is fraught, given the differences between databases. For instance, while the TVT Registry analyses have included all-comer, consecutive bicuspid TAVIs regardless of whether they had other procedures at the same time, the current analysis from the STS Adult Cardiac Surgery Database included only those undergoing isolated index SAVR, which meant that only about 15% of all bicuspid patients in the database were represented.
“What needs to happen is we need to do a randomized clinical trial where we capture the whole scenarios of bicuspid patients,” Makkar said. “We need to do a SYNTAX-like study where we take patients with bicuspid AS, the heart team will randomize these patients, and then we look at the outcomes. Anything else is flawed and subject to selection bias.”
L.A. McKeown is a Senior Medical Journalist for TCTMD, the Section Editor of CV Team Forum, and Senior Medical…
Read Full BioSources
Hirji SA. Benchmarking outcomes of surgical aortic valve replacement for aortic stenosis in patients with bicuspid aortic valves: an analysis of the Society of Thoracic Surgeons Adult Cardiac Surgery Database. Presented at: STS 2022. January 30, 2022.
Disclosures
- Hirji and Kaneko report no relevant conflicts of interest.
- Makkar reports grant/research support and consulting fees/honoraria from Edwards Lifesciences, Abbott, Medtronic, and Boston Scientific.
- Nguyen reports serving on the speaker’s bureau for Edwards Lifesciences.





Comments