TAVI Outcomes Similar in Low-Risk Bicuspid, Tricuspid Aortic Stenosis at 1 Year
Longer-term data in the bicuspid subset are still needed, while debate continues about how an RCT versus surgery might work.

MIAMI, FL—When carefully selected, patients with bicuspid aortic valves and low surgical risk can do as well with TAVI as patients with three leaflets at least through 1 year of follow-up, according to two registry studies presented here at TVT 2021.
In a study of patients implanted with a self-expanding Evolut R or PRO (Medtronic), the rate of death or disabling stroke at 1 year was 1.4% in patients with bicuspid valves and 2.8% in those with tricuspid valves (P = 0.413), John Forrest, MD (Yale School of Medicine, New Haven, CT), reported. Rates of other outcomes did not significantly differ either.
And in another study of patients who underwent TAVI with a Sapien 3 valve (Edwards Lifesciences), there was no difference in the rate of death, stroke, or CV rehospitalization between the bicuspid and tricuspid groups through the first year (10.9% vs 10.2%; P = 0.80), Mathew Williams, MD (NYU Langone Health, New York, NY).
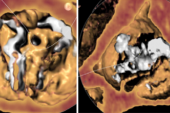
“What we saw is that the outcomes were nearly identical” in the bicuspid and tricuspid groups, with very low overall rates of moderate-or-worse paravalvular leak, Forrest told TCTMD. “I think that goes along with what we’ve seen out of the registries, and that’s really that it probably is not whether the valve is bicuspid or not that makes the big difference in short- and medium-term outcomes as it relates to patients undergoing TAVI. It probably has more to do with the calcium distribution . . . than with whether the native leaflet has two cusps or three cusps.”
He and others stressed, however, that these results were obtained in highly selected populations after patients with unfavorable characteristics were excluded. No low-risk study, in those with bicuspid valves or not, has enrolled an all-comers population, Forrest pointed out.
“I think it’s important when you’re looking at any low-risk study [to] recognize that there are a handful of patients who were excluded because of anatomic features and there also is the potential for site selection bias,” he said.
Responding to the two new presentations, cardiac surgeon Gorav Ailawadi, MD (University of Michigan, Ann Arbor), told TCTMD he was “thrilled to see this data. I think it’s much better than any surgeon would have thought it would be” in patients with bicuspid valves, who were excluded from the pivotal TAVI trials.
But he agreed that the careful selection of patients for these studies is an important issue to consider when viewing the results. One of the concerns some have had about performing TAVI in patients with bicuspid valves, he explained, is that if regulators ultimately approve this indication, out in broader practice there will not be the same degree of attention paid to some of the factors that make a patient a good or bad potential candidate for the transcatheter procedure, he explained. Those include features like annular size and calcium burden.
Physicians also need to be cautious about choosing TAVI over SAVR considering that many patients with bicuspid valves are relatively young and thus may be looking at additional interventions in the future, and that there are no long-term or randomized data to inform how TAVI performs in this subset, Ailawadi said. The selection of TAVI or surgery “really should be done in a heart team approach,” he underscored.
Forrest echoed that point: “Regardless of the number of leaflets, vigilant case planning and a focus by the heart team on the CT angiography is critical for success for these low-risk patients.”
Evolut R or PRO
The main outcomes of the single-arm, 150-patient Low-Risk Bicuspid Study, reported last year, demonstrated a low rate of all-cause mortality or disabling stroke (1.3%) at 30 days after TAVI with an Evolut R or PRO prosthesis performed at 25 US centers.
For the 1-year analysis, Forrest and colleagues propensity-matched patients from this study with those from the TAVI arm of the Evolut Low-Risk Trial, all of whom had tricuspid aortic valves, resulting in 145 patient pairs. Before matching, bicuspid patients were younger and more likely to be women and to have undergone a prior PCI compared with the tricuspid group.
Those differences were no longer seen after matching, although the bicuspid patients were more likely to undergo preimplant balloon valvuloplasty (91.7% vs 29.7%) and to have embolic protection deployed (29.7% vs 1.4%; P < 0.001) and were less likely to have resheath or recapture performed (32.4% vs 44.8%; P = 0.03). Rates of device success, correct positioning of the valve, and the early absence of moderate or severe prosthetic regurgitation were similarly high in both groups.
A look at clinical outcomes showed “results that we’ve come to expect for tricuspid valves being seen with bicuspid valves,” Forrest said.
As at 30 days, there were no differences at 1 year in death or disabling stroke, major bleeding (1.4% vs 2.8%), pacemaker implantation (16.6% vs 17.9%), aortic valve-related rehospitalization (3.5% vs 4.9%), or valve thrombosis (1.4% vs 0.7%; P = NS for all).
Hemodynamics improved to a similar extent in both the bicuspid and tricuspid groups. And paravalvular regurgitation, which was an early concern with doing TAVI in patients with bicuspid valves, was similar in the two groups. At 1 year, in fact, the rate of moderate or severe regurgitation was lower in the bicuspid group (0.8% vs 3.9%; P < 0.001), which might have to do with the fact that the registry patients were treated at a later time point and operators may have been more comfortable with the prosthesis, Forrest said.
“The presence of a bicuspid valve does not appear to impact procedural or early outcomes at 1 year in low-risk patients undergoing TAVR using a self-expanding supra-annular valve,” he concluded during his presentation.
Sapien 3
Williams presented a similar analysis that propensity-matched patients included in the PARTNER 3 Bicuspid Registry and Bicuspid Continued Access Protocol (CAP) Registry with tricuspid patients randomized to TAVI in the PARTNER 3 trial, leaving 148 pairs with low surgical risk.
After matching, there were no differences between groups in terms of baseline clinical characteristics, but bicuspid patients had larger annuli (486.0 vs 457.1 mm2; P = 0.01) and a longer procedure duration (64.0 vs 50.0 min; P < 0.01).
At 1 year, there was no difference in the rate of the primary composite endpoint of death, stroke, or CV rehospitalization or in the rates of the individual components or pacemaker implantation (P = NS for all):
Death (0.7% vs 1.4%)
- Stroke (2.1% vs 2.0%)
CV rehospitalization (9.6% vs 9.5%)
Pacemaker implantation (6.8% vs 7.4%)
Improvements in hemodynamics, NYHA class, and quality of life were similar in both groups, and there were no differences based on the number of leaflets in terms of paravalvular regurgitation at 30 days or 1 year.
Williams acknowledged several limitations, including the lack of longer-term data; the highly selected patient population, which means the conclusions may not be generalizable to all bicuspid morphologies; and the fact that echocardiographic data were site-reported in the CAP Registry.
Longer-term follow-up will be needed to confirm the results, he said.
Patient Selection and the Need for Randomized Data
Asked during a panel discussion after his presentation where research should go next, Forrest said that there is now a good understanding of which populations can be treated with TAVI with good results and which cannot be—patients with heavy calcification in the LV outflow tract, which increases risks of paravalvular leak and annular rupture, for instance. “I think it makes sense in low-risk patients that we’re not putting them in,” he said. “They’re probably better off with surgery.”
Alluding to the lack of randomized evidence showing how TAVI fares against surgery in low-risk patients with bicuspid valves, Forrest said the real question is what a randomized study would look like. He asked whether it would be worth randomizing the same types of highly selected patients that were included in these propensity-matched analyses. “I’m not sure it is, because we know the results here,” said Forrest.
On the other hand, it might make sense to perform an RCT in a less-selected, all-comers population of patients with bicuspid valves or in patients with higher surgical risk, he added.
Several panelists expressed skepticism about the feasibility of performing an RCT in a low-risk, bicuspid population at this point, but Ailawadi said there is still a need to push for more data. A randomized trial is ideal, especially when talking about a younger patient population with bicuspid valves, he said.
“If we really want to move the needle and prove it, we would do a randomized trial,” he said, adding that follow-up would have to be much longer than it was in prior TAVI trials to ensure good long-term outcomes relative to surgery. “The challenge is not that we can’t find patients. I think the challenge is we have to be willing to wait 5 or 10 years for results.” He agreed with others that a trial would have to include all-comers rather than the highly selected populations included in observational studies up to this point.
For now, he said, “data like this is supportive and it helps to shift the needle somewhat. But I think we still have to be cautious and really be thinking about the exclusions. Obviously the things that they used to exclude—like the anatomic criteria—need to be put into practice and a lot of bicuspids still have those—over half [of patients] in those studies.”
And when considering a relatively young patient—say, under 65 or 70—physicians need to keep their focus on management over the remaining lifetime, and not just the procedure at hand, Ailawadi said. “If we model what a TAVR will look like now, and if it doesn’t look like we can do a TAVR after that without some concern about the coronary anatomy, then we’ll end up offering them a surgical AVR.”
Another factor to consider as well, Ailawadi said, is the rate of pacemaker implantation after TAVI, which was much higher in both registry studies—regardless of the number of leaflets—compared with what has been seen with surgery. “We think it’s benign, but we’re also learning the long-term impact of pacing is maybe detrimental, and secondly, the impact on the tricuspid valve can be very devastating long term with a pacemaker in.”
Because these bicuspid patients are often young, “we need to be thinking about a lifetime approach, which often means SAVR first and then TAVR after that,” Ailawadi said.
For Forrest, it’s critical for patients to play a role in the treatment decisions. “There’s a lot of things to weigh with the patient, and I think [we need] a true shared decision-making process with the patient where they’re aware of what data exists and also what data doesn’t exist so that they can make an informed decision. . . . I really think if they’re a candidate for both, it should be the patient driving that with the physician providing the patient with the information they need to make an informed decision.”
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Forrest J. Comparison of 1-year outcomes after transcatheter aortic valve replacement between low-risk patients with severe bicuspid and tricuspid aortic stenosis. Presented at: TVT 2021. July 20, 2021.
Williams M. The PARTNER 3 bicuspid registry for Sapien 3 TAVR in low-risk patients. Presented at: TVT 2021. July 20, 2021.
Disclosures
- The Low-Risk Bicuspid Study was sponsored by Medtronic.
- Forrest reports grants/research support and consulting fees/honoraria from Edwards Lifesciences and Medtronic.
- The PARTNER 3 analyses were funded by Edwards Lifesciences.
- Williams reports financial support from Boston Scientific, Edwards Lifesciences, HLT Medical, and Medtronic and other relationships with Micro Interventional Devices and Thubrikar Aortic Valve.
- Ailawadi reports receiving consulting fees/honoraria from and/or serving on the speakers bureau for Abbott Vascular, Admedus, Edwards Lifesciences, Medtronic, and WL Gore & Associates.



Comments