For Cardiac CT, COVID-19 Has Toppled Silos and Paved the Way for Change
A session at the SCCT virtual meeting explored the evolution of CT during the pandemic and expectations for the future.
The COVID-19 pandemic has upended the field of cardiac imaging and will lead to lasting changes in education, efficiency, and collaboration, experts predicted during a dedicated session at the 2020 Society of Cardiovascular Computed Tomography (SCCT) virtual meeting.
Many of the issues brought up during the session existed prior to COVID-19, according to SCCT’s outgoing president Ron Blankstein, MD (Brigham and Women's Hospital, Boston, MA). “But I think in the COVID era, where we are trying to be as efficient as possible, it's even more important to always ask: what is the best test to address the question so we can rapidly and efficiently provide the right answers?”
Quick Adaptation
Providing an overview of the pandemic and the current state of cases and mortality rates, James Town, MD (University of Washington, Seattle), said that while the medical field has been forced to evolve, “we can't abandon our core values.” COVID-19, he noted, has “accentuated disparities in our communities” and should serve as a reminder to physicians to examine their individual processes of care to achieve better racial equity.
In the COVID era, where we are trying to be as efficient as possible, it's even more important to always ask: what is the best test to address the question so we can rapidly and efficiently provide the right answers? Ron Blankstein
“Secondarily, I think we need to start asking now what survivorship looks like in terms of quality of life as well as economic recovery in the face of an injured economy,” Town said. “We have seen a rapid evolution of the way evidence-based medicine is developed, disseminated, and implemented. I never would have thought I would be giving a talk where I'm using preprint publications and Twitter data, but I think that's where we are now, where things are getting released to the public pretty quickly before they're in print.”
This quick adaptation will be worthwhile in both responding to the pandemic as well as evolving cardiovascular care, he said.
CT Over TEE
In his talk, Andrew Choi, MD (The George Washington University, Washington, DC), outlined when to optimally use cardiac CT in lieu of TEE, especially as the pandemic continues to unfold.
Given the fact that TEE is an aerosolizing procedure, especially during extubation, early guidance discouraged its use, he explained. “The ideal cardiac imaging test amidst this crisis is something that we need to use just for the most urgent indications, that we want to use for those who have symptoms, that really reduces PPE and resource use, . . . is accurate, and will allow us to change management,” Choi said.
Cardiac CT enables operators to be physically further away from the patient and, unlike TEE, doesn’t require full PPE in patients who are COVID-negative.
Additionally, Choi pointed to a recent study showing a high rate of injury associated with TEE in structural heart interventions. “It highlights what has been suspected and known from the surgical literature: that while TEE as a procedure is incredibly important, particularly in the interventional space, and it's something that I do, I think we have to be mindful of some of these risks that are associated with it.”
CT, on the other hand, has high spatial resolution, allows for full 3-D reconstruction and postprocessing, and is a good option for patients who have known esophageal disease or are frail, Choi said. “Importantly, CT will enable a reduction in PPE use, resource utilization, and is safer.”
“In the postpandemic phase, which I hope is soon, while utilization might revert back to usual practice, I hope—and I hope all of you do as well—that highly efficient, cost-effective, and accurate CT approaches should ideally remain the first line of care,” Choi concluded.
Challenges and Opportunities
Turning in his presentation to the broader use of coronary CT angiography (CTA) during the COVID-19 pandemic, Blankstein argued that its role is broadly dependent on the state of disease—acute or chronic.
Coronary CTA may be useful for differentiating between acute coronary syndrome or myocardial injury, he explained. “This is an important question because 10-30% of patients with COVID who are admitted have elevated troponin markers.” In the early days of the pandemic, physicians were quickly discovering that despite presenting with ST-elevation and elevated enzymes, many COVID-positive patients did not have coronary disease, but rather myocardial injury. “Particularly as we were trying to limit the use of PPE in the cath lab, the question that arose in the field of cardiac CT was: When should we be using cardiac CT? And it wasn't a very straightforward or easy question to answer actually,” Blankstein recalled.
Current SCCT guidance states that CTA can be used in selected patients to exclude obstructive coronary disease only when diagnostic quality imaging can be achieved, Blankstein said. “And this is important because not all patients with elevated enzymes are going to be good candidates for coronary CTA. So we have to be selective.”
But when patients have equivocal symptoms or even an atypical ECG, it would be “reasonable to consider coronary CTA together as part of a joint conversation with our interventional cardiology colleagues,” he observed, a stance also supported by a recent, multispecialty guidance document. “When we look at the European guidance statement, it states that in patients with acute chest pain and suspected obstructive coronary disease, CTA is the preferred noninvasive imaging modality since it is accurate, fast, and minimizes the exposure of patients.”
For patients with acute chest pain but elevated enzymes, a population that has been lacking in most CT research, it’s likely that a CT would not be warranted over another test like invasive angiography, Blankstein said. Some guidance for this population comes from the recent VERDICT trial—which showed that among ACS patients, most with elevated enzymes, 30% did not have any stenosis and CT had a high negative predictive value for excluding obstructive disease.
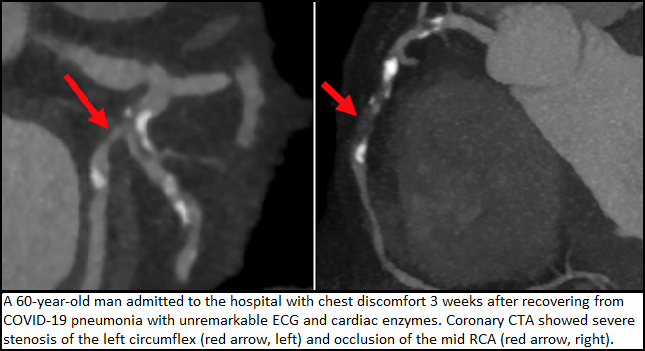
Blankstein presented two varying case uses of coronary CTA during the pandemic. One was in a 22-year-old COVID-positive patient who presented with elevated troponins and chest discomfort who turned out to have no plaque and no stenosis. “Of course, this is one end of the spectrum, a patient that perhaps coronary CTA is relatively easy to do,” he said. The other case was of an 87-year-old patient admitted to the hospital with COVID pneumonia who had suspected stress-induced cardiomyopathy. “The reason why I was not excited to do a CT was that this was a patient who was tachycardic, was on a ventilator, had his arms down, and because of his hemodynamic instability, we could not administer beta-blockers. So certainly not the ideal patient for a CT.”
Going forward, Blankstein said, it’s likely that CT will be used more often in the chronic phase of disease “to evaluate patients who now have chest discomfort, perhaps new LV dysfunction, or new arrhythmias.”
Per a recent statement, “when there is a clinical suspicion of coronary disease, CT, MRI, and nuclear all have important roles, but specifically the role of CT . . . is evaluating patients with no known coronary disease who have symptoms of possible angina, or to identify patients with coronary disease who can be treated conservatively,” he explained.
Finally, CTA will remain a vital tool for patients who are COVID-negative, Blankstein concluded. “In fact, this will continue to be the most common group of patients that all of us will evaluate. And in this particular setting, CTA will be helpful for avoiding unnecessary hospital admissions, for avoiding invasive angiography, and for identifying patients who actually have coronary disease, in whom we can treat them conservatively because they have no high-risk anatomy or perhaps [CT-fractional flow reserve that] shows no flow-limiting disease.”
Role of Diagnostic Testing
Also during this session, Jonathon Leipsic, MD (St. Paul's Hospital, Vancouver, Canada), spoke to the impact of COVID-19 on diagnostic testing. Calling the pandemic a “crucible for change,” he said the current period highlights the need to “do the right test at the right time for the right patient, and we shouldn't just follow our historical algorithms for workup and management of patients because that's what we used to do. And we certainly need to be avoiding layering of testing when at all possible.”
As illustrated in a multisocietal document published last month in the Journal of the American College of Cardiology, Leipsic pointed out that “we shouldn't be thinking of this COVID pandemic as really one environment in which we're practicing. . . . Clearly how we test and how we approach testing in patients will very much depend on the overall community spread and the disease burden in the populations we're serving. I think this document, while high level, really does drive that home.”
This pandemic and the expectation of our patients and the Hippocratic oath really behooves us that we ignore historical pathways and we really focus on what makes most sense for our patients. Jonathon Leipsic
The pandemic has also shown the value of using CT beyond its traditional applications, particularly given the potential to apply machine learning to large data sets. “What we're realizing more and more is that in the era of COVID, if we have acquired a data set, whatever the imaging modality, . . . we really can't leave any so-called data on the table. We need to explore it for all its potential use,” Leipsic stressed, adding that this can be applicable in guiding transcatheter mitral interventions, understanding leaflet morphology, and planning left atrial appendage closure, among other clinical scenarios. “Historically we may have wanted to do two tests, but perhaps now we have to consider getting by with just one and one that doesn't involve invasive procedures and doesn't risk aerosolization.”
He urged imagers to continue to encourage interventional cardiologists to appreciate the potential benefits of CTA, particularly in the context of COVID-19 when they don’t want to be taking unnecessary patients to the cath lab who won’t derive a benefit.
“Ultimately, while I am obviously very zealous about the opportunities of cardiac CT broadly but certainly in the contest of COVID, I think we do need to reflect that we always need to follow best practice and follow the appropriate use guidelines,” Leipsic concluded. “Particularly in the era of COVID, we shouldn't be layering tests. We should do the test that answers the question. We should avoid CCTA in known disease, avoid it in the setting of extreme [coronary artery calcium] perhaps, avoid it also in poorly controlled heart rate, and then ultimately we really need to support that we do the right test to answer the clinical question as safely, accurately, and cost-effectively as possible. And I think for many of those questions, cardiac CT will be the test that provides those answers.”
Lasting Changes
In a panel discussion following the presentations, session co-moderator Todd C. Villines, MD (University of Virginia, Charlottesville), agreed with Leipsic that the pandemic should spur change in the field, and in fact already has. “At my own institution, it has been exactly that to where we've taken patients who we would have sent directly to the cath lab and ask questions later, and now my interventionalists come to me and say: ‘Would you please do a coronary CT in this patient?’” he said. “We've moved almost entirely to using CT for appendage clearance, et cetera, and we've been doing that for a while.”
He asked the panel what they think will be the biggest enduring change to the practice of cardiac CT as a result of the COVID-19 pandemic.
Blankstein replied that delivery of education has already changed permanently given the need for virtual offerings when travel stopped being an option. “On the clinical front, we are just going to have much more appreciation for tests that are efficient, that answer a question quickly and get people out of the hospital,” he said. “Efficiency in throughput, in safety are things that I think we are going to value for a long time and those are things that are all things that cardiac CT can offer.”
Choi said the increased need for teamwork will likely last beyond the span of the pandemic. “All of us are learning at our institutions. There's been increased collaboration across different physicians, departments because of the pandemic, and I think it's been really one nice aspect of how we deliver care,” he said. Also, “if you're a program that needs to change the equipment or change how the program is structured, this is a time to do that and this is an opportunity for us to expand the field because the pandemic demands it of us. We can't idle in legacy approaches, because they're not the most effective or the safest.”
Leipsic agreed, adding that the current state of the world has led to the dismantling of traditional silos within medicine and especially cardiac imaging. “This pandemic and the expectation of our patients and the Hippocratic oath really behooves us that we ignore historical pathways and we really focus on what makes most sense for our patients.”
Photo Credit: Ron Blankstein
Yael L. Maxwell is Senior Medical Journalist for TCTMD and Section Editor of TCTMD's Fellows Forum. She served as the inaugural…
Read Full BioSources
Town J. The evolving epidemic of COVID-19: adapting under pressure. Presented on: July 17, 2020. SCCT 2020.
Choi AD. When is cardiac CT a good alternative to TEE. Presented on: July 17, 2020. SCCT 2020.
Blankstein R. Opportunities and challenges for coronary CTA during the COVID-19 pandemic. Presented on: July 17, 2020. SCCT 2020.
Leipsic J. Impact of COVID on diagnostic testing. Presented on: July 17, 2020. SCCT 2020.
Disclosures
- Town and Villines report no relevant conflicts of interest.
- Choi reports holding stock in Cleerly.
- Blankstein reports receiving grants and research from Amgen and Astellas.
- Leipsic reports receiving grant support from CIRH, NIH, GE Healthcare, and Heartflow; serving as a consultant for Heartflow and Circle CVI; core lab for NIH, Edwards, Neovasc, Tendyne, Abbott, Medtronic, and Pi Cardia; and holding stock options in Circle CVI and Heartflow.
- Parwani reports serving as a consultant to Brilanta.


Comments