CCTA in Patients With Prior CABG Cuts Complications of Invasive Angio: BYPASS-CTCA
One researcher calls this practice a “no-brainer” but acknowledges that not everyone will have access to CT.
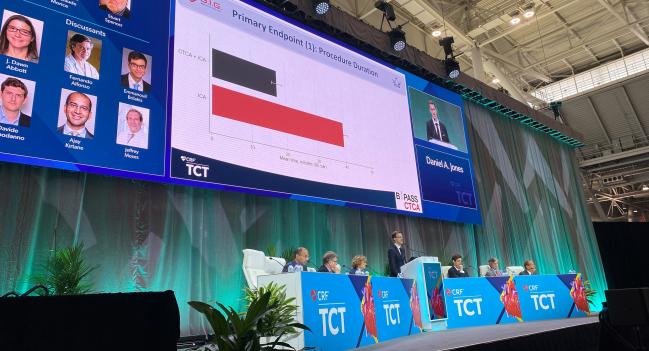
BOSTON, MA—Adjunctive coronary CT angiography (CCTA) prior to invasive coronary angiography in patients who’ve had prior CABG shortens procedure duration, improves patient satisfaction, and lowers rates of contrast-induced nephropathy (CIN) as well as procedural complications and MACE at 12 months, according to new randomized data.
“If it's logistically feasible, then doing a CT makes a lot of sense,” said Daniel Jones, MD, PhD (Queen Mary University of London, England), who presented the findings during a late-breaking clinical science session at TCT 2022, told TCTMD. He acknowledged that not all centers may have access to CT, especially for same-day patients with ACS, but called this practice a “no-brainer” if the machines are available.
The findings stand somewhat in contrast with those of the GREECE trial, which, as reported by TCTMD, showed that CCTA prior to invasive coronary angiography actually increased the amount of contrast used, although it did not increase the amount of CIN.
“The main difference is essentially [that GREECE] was a very small study [with approximately] 80 patients in each arm and it wasn't powered for any endpoint except for contrast,” Jones said. “We powered our study off the consequences of contrast, so contrast-induced nephropathy and procedure duration and satisfaction. . . . They also used older-generation CT scans and they admitted to that at the time.”
In a press conference, Ori Ben-Yehuda, MD (Cardiovascular Research Foundation, New York), called this a “really beautiful study.” He said: “It’s been my practice to do this, but it's always better to have real data.”
Procedural Improvements With CCTA
For the study, Jones and colleagued randomized 688 patients (mean age 70 years; 84% male) with prior CABG to invasive coronary angiography alone (n = 344) or preceded by CCTA (n = 344). Roughly 45% of patients overall presented with ACS, and there was a high burden of comorbidities with 85% of patients having hypertension, 48% with prior PCI, and 68% with prior MI. The mean number of bypass grafts in both arms was around 1.2.
Compared with patients who had invasive coronary angiography alone, those who underwent adjunctive CCTA had shorter procedure durations (mean 17.4 vs 39.5 min; OR -22.12; 95% CI -24.68 to -19.56), less CIN (3.2% vs 27.9%; P < 0.0001), and 40% greater patient satisfaction on a questionnaire with a 5-point scale where 1 is satisfied and 5 is not (1.49 vs 2.54).
Significantly less contrast was used for patients who underwent CCTA before their procedures (mean 77.4 vs 173 mL), and radial access was used more frequently (76.85% vs 56.73%; P < 0.001 for both). Also, while only a single patient in the CCTA arm had at least one graft not evaluated because it couldn’t be located or was assumed occluded, 24.27% of the patients who did not have CCTA fell into this category.
There was also an 80% reduction in procedural complications with adjunctive CCTA (2.4% vs 10.8%; P < 0.001), with significant reductions seen for both periprocedural MI (0.58% vs 6.43%; P = 0.001) and vascular access complications (0.58% vs 4.39%; P =0.007).
At 12 months, MACE was lower for those who underwent CCTA (16.28% vs 29.36%; adjusted OR 0.44; 95% CI 0.30-0.64), driven by significantly lower rates of nonfatal MI (9.59% vs 18.60%; adjusted OR 0.44; 95% CI 0.28-0.70). Cardiovascular mortality (1.74% vs 3.78%; P = 0.079) and unscheduled revascularization (5.81% vs 9.30%; P = 0.092) also trended lower with preprocedural CCTA.
‘Astounding’ AKI Rate
In discussion following the presentation, Jeffrey Moses, MD (NewYork-Presbyterian/Columbia University Irving Medical Center, New York, NY), called the rate of acute kidney injury in the non-CCTA arm “astounding.” He questioned whether that contributed to the “sharp division in MACE over the long term.”
“We were surprised by the rate of AKI in the control group,” Jones replied. “I think the patient groups were relatively high risk, despite their baseline renal dysfunction. There's high rates of diabetes, there were a high proportion of elderly patients in the group, and 27% isn’t out of proportion for published literature of similar high-risk patient groups, although it is, I admit, at the high end.”
He added that the study wasn’t powered to show a difference in MACE, but said, “I think there were a lot of signals to suggest that maybe a reduction in MACE over 12 months isn’t something that's surprising. We had reduced rates of procedural complications, less vascular access, less contrast-induced nephropathy, greater completeness of diagnostic information, which arguably might suggest complete revascularization. So I think there’s enough signal there to suggest that CT might lead to a benefit, but I think we probably need more studies to confirm that.”
If it's logistically feasible, then doing a CT makes a lot of sense. Daniel Jones
Panelist J. Dawn Abbott, MD (Brown University, Providence, RI), asked whether the timing of the CCTA before the procedure might “be an issue for inpatients, even though the venous contrast may not be as renal toxic.”
Jones said stable patients typically had their scans 1-2 weeks ahead of time “because we had time to plan it.” In ACS patients, on the other hand, “the CT was either performed the day before of the angiogram or the day of the angiogram.” He added that while they have not yet conducted an analysis to see if there was an interaction between same-day CCTA and acute kidney injury, “we didn't see any rates of AKI associated [with] the elective CT and the angiogram.”
The study protocol didn’t “mandate how operators use the information from CT” but suggested that occluded grafts not be reengaged, Jones explained. “Whether a patent graft was imaged at angiography, there was variable practice. My personal practice tends to be I would only select a vein graft on invasive angiography if it was diseased on CT or if the native conduit supplied, say, a retrograde collateral for CTO.”
There were a “large proportion” of patients in the CCTA group who didn’t have grafts invasively imaged, he continued, “which I think explains why there was such an impressive difference in terms of procedural duration, contrast amount, and outcomes. But that wasn’t protocolized as part of the study.”
Panelist Ajay Kirtane, MD (NewYork-Presbyterian/Columbia University Irving Medical Center), commented that “many of us have been in this circumstance where we don't know how many grafts there are, we don't know where they're supplied, and we’re looking for cath reports and op reports and that sort of thing. In many respects, this is a nice proof of concept in that way,” he said.
Kirtane agreed that the risk of CIN “seems way striking and needs some more elucidation.” However, he noted, “from a practical standpoint, sometimes we find ourselves getting CTs after the fact. So perhaps doing it up front, especially in cases which are less clear, makes a lot of sense.”
Panelist Davide Capodanno, MD, PhD (University of Catania, Italy), complimented the researchers on using a patient-reported outcome measure as a primary endpoint. “This is a trend that we're seeing more and more in trial design,” he said. “Of course, I feel that patients are happier when you do more diagnostics because they feel, of course, that they are well managed in a way.”
He questioned whether preprocedural CCTA would be cost-effective. “I suspect that this strategy would be favorable because you have less days hospitalized because of contrast-induced nephropathy,” Capodanno said. “But was that considered to have cost-efficacy? Because with two diagnostics here, of course, the cost of the hospitalization would increase.
While he does not yet have cost-effectiveness data, Jones said it will be interesting to look at “because arguably we did potentially prolong some of the inpatient stay in the ACS group,” he said. “So, if someone had a CT and then an angiogram the next day, then that would have prolonged by 24 hours. I suspect it would be cost-effective, but there will be a proportion of patients who will have had their stay prolonged.”
Yael L. Maxwell is Senior Medical Journalist for TCTMD and Section Editor of TCTMD's Fellows Forum. She served as the inaugural…
Read Full BioSources
Jones D. The BYPASS-CTCA study: a randomised controlled trial assessing the value of computed tomography cardiac angiography (CTCA) in improving patient-related outcomes in patients with prior CABG undergoing invasive coronary angiography. Presented at: TCT 2022. September 19, 2022. Boston, MA.
Disclosures
- Jones reports no relevant conflicts of interest.




Comments