CLASP 2-Year Data Promising for Pascal Transcatheter Mitral Repair
Observers caution, however, that a single-arm study can’t predict how another TEER device would compare with the MitraClip.
Preliminary 2-year results from the single-arm CLASP study show that mitral valve repair using the Pascal transcatheter system is associated with high rates of survival and freedom from rehospitalization as well as a durable reduction in mitral regurgitation (MR).
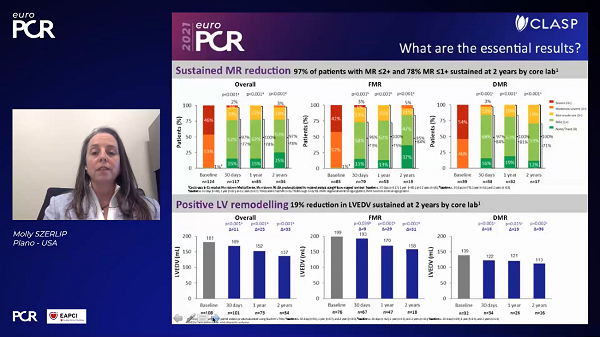
According to Molly Szerlip, MD (Baylor Scott & White Health, Plano, TX), who virtually presented the study as a late breaker at EuroPCR 2021, the data look “extremely good,” at least for the numbers of patients followed so far, in both functional and degenerative MR.
“This reiterates that this is an excellent device and one that needs to be out on the market,” she told TCTMD. “And as the long-term data come out, there's nothing that would make us think that [this device] is not going to continue to have excellent long-term outcomes.”
The 2-year CLASP safety and feasibility results were simultaneously published in JACC: Cardiovascular Interventions.
The Pascal system (Edwards) is still investigational in the United States, where sites are currently enrolling patients into the pivotal CLASP IID/IIF trial. In that study, patients with severe functional or degenerative MR are being randomized to the Pascal or to the MitraClip (Abbott) which is the only transcatheter edge-to-edge repair (TEER) device approved in the United States.
Pascal, as the investigators explain in the paper, has a number of “differentiated” features from the MitraClip, including two clasps that grasp the mitral leaflets with the paddles facilitating coaptation, then a central spacer that helps to fill the regurgitant orifice area. The clasps can be operated in tandem or independently, which allows for staged leaflet capture and adjustment—a particularly attractive and novel feature of this device when it was first launched. MitraClip, by contrast, was originally designed with simultaneous leaflet capture only, although the latest G4 device now offers independently controlled “grippers.”
Early Optimism
The CLASP safety and feasibility study enrolled a total of 124 patients with clinically significant MR (≥ 3+) and NYHA class II-IVa who were deemed suitable for edge-to-edge repair. More than two-thirds of the cohort (69%) had functional MR, and more than 60% were NYHA class III or IV. Earlier results—including the primary endpoints of procedural success, clinical success, and MACE at 30 days, as well as additional 1-year results—were presented at TCT 2020 and have been previously published in JACC: Cardiovascular Interventions.
As Szerlip showed at EuroPCR this week, 48 out of the original 124 patients have reached the 2-year follow-up mark. In this incomplete group, Kaplan-Meier estimates pointed to survival rates of 80% (72% in the functional group and 94% in the degenerative group). Freedom from heart failure hospitalization was 85% (81% for functional, 98% for degenerative). In terms of MR reduction and associated heart function, 78% of patients had MR grades of less than or equal to 1+ at 2 years and this was accompanied by improvements in left ventricular end-diastolic volume and NYHA functional class, with 93% of patients now in NYHA class I or II.
There's nothing that would make us think that [this device] is not going to continue to have excellent long-term outcomes. Molly Szerlip
These signs of ventricular remodeling are “kind of what we all hope for, for any device,” Szerlip stressed to TCTMD. “You want there to be remodeling of the LV so that the function improves, and we definitely see that with this device.”
Wrapping up her EuroPCR presentation, Szerlip concluded: “The Pascal transcatheter valve repair system is a favorable option for treating patients with MR. . . . We are excited and awaiting the CLASP IID/IIF randomized clinical trial.”
Asked about progress in that pivotal trial, Szerlip estimated that investigators are about halfway through the enrollment process—COVID-19 having slowed down the trial, although it’s back to full speed now, as centers open up. That means full trial follow-up results are still a number of years away.
“But the data for the 2-year outcome is very good for both rehospitalization and mortality,” she stressed, and the device itself is easy to use, “at last as good or better than the MitraClip” and “not as bulky” or “rigid.”
Wait and See
Commenting on the results for TCTMD, Anita Asgar, MD (Montreal Heart Institute, Canada), cautioned that it’s too soon for comparisons with the MitraClip, since CLASP was not a head-to-head study.
“I would say that these results are very reassuring for the field of repair, because what it's showing us is that edge-to-edge repair is definitely something that can be successful, regardless of whether its MitraClip or Pascal,” Asgar said.
She took issue, however, with some of the emphasis placed in the paper, particularly with regards to LV function and heart failure hospitalizations which she characterized as a bit of a stretch, since these were not prespecified endpoints in the CLASP safety and feasibility trial.
These results, are “another plus for the field of mitral valve repair, but other than that, I don't think there's anything more we can say, we really do have to wait for randomized trials because I think some of the comparisons they make here are premature, unfair, and not particularly balanced.”
Likewise, Georg Goliasch, MD, PhD (Medical University of Vienna, Austria), who wrote an editorial accompanying the published CLASP results, told TCTMD that it’s not yet possible to imagine how Pascal might be positioned alongside the MitraClip, or whether one device might have a particular niche or advantages over the other.
“There are currently insufficient data to answer these questions,” he told TCTMD in an email. “As both devices are edge-to-edge repair systems targeting similar lesions there might be significant overlap in this particular patient population,” particularly since some of the differentiating factors between devices are disappearing in newer iterations. “The Pascal device may offer a leaflet repair with decreased mechanical leaflet traction, [which is] specifically appealing to treat ventricular secondary MR because mechanical forces applied to leaflets remain low, and the spacer augments the leaflet surface in a way that reduces restrictive diastolic opening,” Goliasch observed. “However, this remains highly speculative.”
Shelley Wood was the Editor-in-Chief of TCTMD and the Editorial Director at the Cardiovascular Research Foundation (CRF) from October 2015…
Read Full BioSources
Szerlip M, Spargias KS, Makkar R, et al. 2-year outcomes for transcatheter repair in patients with mitral regurgitation from the CLASP study. J Am Coll Cardiol Intv. 2021;Epub ahead of print.
Goliasch G, Bartko P. Durable reduction of mitral regurgitation after 2 years: another ace up the TMVR sleeve. J Am Coll Cardiol Intv. 2021;Epub ahead of print.
Disclosures
- Szerlip reports consulting or honoraria from Edwards Lifesciences.
- Asgar reports consulting from Abbott and Edwards Lifesciences.
- Goliasch reports no relevant conflicts.




Comments