Clips and Rings for Tricuspid Regurgitation: Early Data Speak to Progress and Challenges
It’s early days for these devices, all of which debuted in the mitral position. Matching the patient to the technology will require more data.
LONDON, England—Results from several small and preliminary studies testing a range of devices for tricuspid regurgitation (TR) hint that percutaneous therapies are making progress for what’s long been called the “forgotten” valve. But not all of the studies, presented here at PCR London Valves 2018, turned out as planned—at least in early results—and the jury is still out as to just how big of a clinical impact these therapies might have and how best to match the right patient to the right device.
“The recurring message that you heard here is that you need to tailor the procedure to the patient’s particular anatomy,” one of the presenters, Neil Fam, MD (St. Michael’s Hospital, Toronto, Canada), told TCTMD. “It’s not just one size fits all,” which is the same cautious approach used in other areas of medicine, he stressed, “and it makes sense to do that with the tricuspid as well.”
Three digital posters, presented on the opening day of the meeting, looked in turn at the Cardioband percutaneous annuloplasty ring (Edwards Lifesciences) and the MitraClip (Abbott) and the Pascal device (Edwards)—both leaflet coaptation devices—in the setting of tricuspid regurgitation.
Cardioband at 6 Months
Azeem Latib, MD (IRCCS San Raffaele Scientific Institute, Milan, Italy), presented 6-month results from TRI-REPAIR, the multicenter, first-in-man trial of the Cardioband system for tricuspid regurgitation, conducted by the device manufacturer (Edwards) to get CE Mark approval in Europe. Thirty-day results were reported earlier this year at EuroPCR 2018 and the Structural Heart Disease Summit, and the device was cleared by European regulators in April 2018.
As Latib explained here, the tricuspid Cardioband system is based on the device originally developed for mitral regurgitation using the same band, the same anchors, but a different delivery system. The percutaneously delivered device is an incomplete, semi-rigid annuloplasty ring with a gap for the atrioventricular (AV) node. TRI-REPAIR, conducted at four European centers, enrolled 30 patients with severe functional TR, 83% of whom had NYHA class III/IV heart failure.
Technical success—defined as successful access, device deployment, and positioning—was 100%, Latib said, but two patients died within 30 days and one of these was deemed device-related. No myocardial infarctions occurred and there were no device-related surgeries, although four patients had bleeding complications, three patients had right coronary artery complications, two patients had ventricular arrhythmias, and one patient had AV block.
At 6 months, annular diameter remained significantly reduced compared with baseline (37.3 vs 43.3 mm; P < 0.001). Other echocardiography parameters also suggested improvements in effective regurgitant orifice area and vena contracta. Six-minute walk test, quality-of-life scores, and NYHA class were all significantly improved from baseline.
While 6 months represents “early experience” with the Cardioband tricuspid system, the reduction in regurgitation appears to be sustained at 6 months, “and is accompanied by clinically and statistically significant improvements in functional status, quality of life, and exercise capacity,” Latib said. “Further studies are warranted to validate the initial promising results.”
PASCAL for TR: Early Signs of Benefit
In a second, even smaller study, Fam presented 30-day results with another Edwards device, the Pascal transcatheter valve repair system. Like the MitraClip, the Pascal was originally designed for mitral regurgitation but has longer, wider paddles, a central spacer which helps plug the coaptation gap, and the ability to independently grasp the valve leaflets, which can help with larger coaptation gaps and severe leaflet tethering, Fam said.
Among the 12 patients treated at three Canadian and European hospitals, clip placement was achieved in 11, with seven patients receiving two clips. A single leaflet detachment was observed, and this patient died of presumed cardiac causes, Fam said. There were no other complications during or following the procedure, including no pericardial effusions, TR worsening, or acute worsening of right ventricular function.
At 30 days, all patients showed improvements in mean TR grade based on a 5-grade scale, falling from 3.9 at baseline to a mean of 1.6. The proportion of patients with TR grade 1 actually improved between postprocedure levels and 30 days, Fam noted.
“Patients with severe TR can be treated with a Pascal device,” Fam concluded. “It can overcome some of the anatomic challenges we face such as large coaptation gaps and leaflet tethering and obviously future studies are needed to further prove the safety and efficacy of this approach.”
MitraClip for TR: No Early Impact on Kidneys, Liver
In the third presentation of the session, Jörg Hausleiter, MD (Klinikum der Universität München, Munich, Germany), presented 30-day results from a series of 135 patients with TR, looking specifically at the impact of MitraClip coaptation on kidney and liver function, which are known to be adversely affected in patients with severe TR.
In this series, the proportion of patients with TR grade ≥ III improved from 95.9% at baseline to 18.2% by 30 days, but that improvement appeared to have no effect on kidney or liver function, using a range of metrics.
In a discussion following his presentation, Hausleiter acknowledged that 30 days is likely too short for any benefits to manifest, but said he was encouraged by other measures of clinical improvement. Nearly all of the patients were in NYHA class III or IV at the study outset, but by 30 days, 60% to 70% of patients were in NYHA class I or II. Six-minute walk test was also significantly improved.
In the future, asked Olaf Wendler, MD (King's College Hospital, London, England), who co-moderated the session, “when we assess the outcome of tricuspid valve repair, what kind of outcomes should we look at at 30 days? Not liver function?”
“Certainly not liver function,” Hausleiter replied. “For me, the cleaner test, which we are doing for assessing heart failure, would be 6-minute walk test. . . . Improvement in the HF questionnaire would be another one. Repeat hospitalizations will be a harder endpoint [to meet],” he continued, “but there are also other metrics and we are presenting some data on that. Activity tracking, for example, which is more representative of daily life, and with this you can see a significant improvement” following tricuspid valve leaflet coaptation, he said.
Which Approach, Which Patient?
Following the two coaptation presentations, session co-moderator, Maurizio Taramasso, MD, PhD (University of Zurich, Switzerland), asked whether it is possible, at this early stage, to know which clip device—the MitraClip or the Pascal—might work better for a patient with TR.
“It’s an important question,” Fam replied. “[The Pascal] device is very good at bridging large coaptation gaps, because you can grasp one leaflet and torque the catheter and pull the leaflet over and join it to the septal leaflet. In 15 out of 18 clips in our study, that strategy was used.”
Fam added that he has also used the latest generation the MitraClip XTR device for tricuspid procedures “and I was impressed.”
“The main difference between the Pascal and the MitraClip is that the width of the arms is double with the Pascal so you can grasp more tissue, but at the same time because it is a wider device, you may have trouble getting between chords to grab the free edge of the leaflets. In the one case where we were not successful [in placing a Pascal clip], the patient had very dense chordae and we were able to come back with a MitraClip NT and do the procedure. So I think there is a different device for different anatomy is the future.”
Wendler, a cardiothoracic surgeon, followed up with a question about the size of the tricuspid annuli in patients with TR, asking whether a leaflet clip is “enough” or if it should be combined with a device like the Cardioband.
“Cardiologists should not assume that we are any smarter than surgeons,” Fam replied, adding that combination procedures may yet prove to be the way of the future. “But again, you need to tailor the therapy to the underlying pathology. If you have severe tethering, annuloplasty will not be very effective and in these cases, most of whom had a lot of tethering, I think leaflet coaptation was the way to go.”
Speaking with TCTMD following the session, Wendler was not persuaded, noting that the surgical experience with functional tricuspid regurgitation suggests that in most cases, “if you do a ring, you fix the problem and you don’t need to do anything else.”
It’s not clear how many patients will present with leaflet tethering or related pathology that would make them suitable for coaptation procedures only. The “vast majority” of patients have annular dilation, Wendler said, “and in those patients, I think the ring is the more promising of these kind of procedures.”
Time and Money
Fam, however, countered to TCTMD that predictions like these don’t take into account the fact that surgeons are not typically operating on the high-risk patients with advanced RV remodeling currently being considered for transcatheter procedures, because of the need for cardiopulmonary bypass.
“The patients we treat are beating-heart procedures with no heart-lung machine,” Fam said. “We’re getting very late-stage patients who are kind of in a desperate situation. So, by definition, we are treating patients who have tethered leaflets and annuloplasty is not adequate to treat that problem. You need a leaflet solution for such patients.”
Asked about combination annuloplasty-plus-clip procedures, Hausleiter pointed out that such a strategy would be both costly and time-consuming: the Cardioband procedures alone are “taking hours” to complete, he said.
“It’s too early to make any conclusions about staged procedures right now, or to say that one procedure is more efficacious than another,” Hausleiter told TCTMD. “We really need to wait and see, after we have more established therapies. Then we can start comparing or thinking about who would benefit more from a combined procedure or who might have a perfect result from a leaflet device. . . . There are things to learn in the next few years before we can really make any statement about what should be the ideal, nonsurgical procedure in the future.”
There are also a number of new devices still in development, including full replacement devices, he added. It remains to be seen which technologies will prove dominant and what different patients have to gain from the various options available down the road.
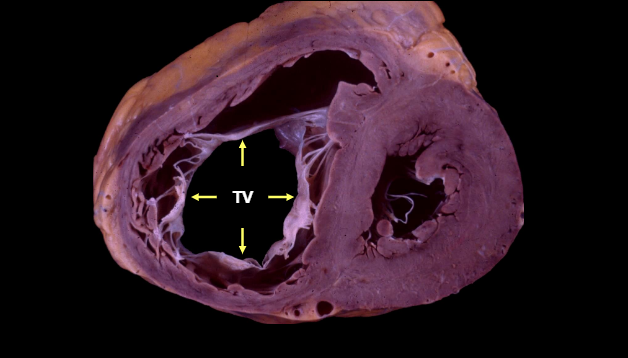
Photo Credit: Adapted from Sarano ME. Impact and natural history of functional tricuspid regurgitation. Presented at: TCT 2016. November 1, 2016. Washington, DC.
Shelley Wood was the Editor-in-Chief of TCTMD and the Editorial Director at the Cardiovascular Research Foundation (CRF) from October 2015…
Read Full BioSources
Multiple presentations. Transcatheter Tricuspid Intervention. Presented at: PCR London Valves 2018. September 9, 2018. London, England.
Disclosures
- Hausleiter reports receiving speakers’ honoraria from Abbott and Edwards.
- Latib, for a previous Cardioband presentation, reported receiving grant/research funding and consulting fees/honoraria from Medtronic, Mitralign, millipede, Amaranth Medical, Valtech Cardio, Spectranetics, Acist Medical, Abbott, Keystone Heart, ICS, InnovHeart, and Mitraltech.
- Fam did not provide a disclosure statement.


Comments