Complete Revascularization Benefits May Be Due to Stenting Vulnerable Plaques
An OCT substudy of the COMPLETE trial shows vulnerable plaques are more common in obstructive nonculprit lesions.
PHILADELPHIA, PA—In patients with STEMI and multivessel disease, the reduction in CV death or new MI achieved in the COMPLETE trial by intervening in obstructive nonculprit lesions after primary PCI might be related to the effect of stenting vulnerable plaques, an optical coherence tomography (OCT) substudy suggests.
Nearly half of patients who underwent OCT imaging during their staged procedure (47.3%) had a thin-cap fibroatheroma (TCFA) detected in an obstructive nonculprit lesion. And obstructive lesions—those with greater than 70% diameter stenosis by visual assessment—were more likely to have a TCFA than were nonobstructive lesions.
Natalia Pinilla-Echeverri, MD (McMaster University, Hamilton, Canada), reported the results here at the American Heart Association (AHA) 2019 Scientific Sessions earlier this week.
“This may explain the benefit of routine PCI of obstructive nonculprit lesions in patients with a STEMI and multivessel disease,” Pinilla-Echeverri said during her presentation. She noted, however, that the study was designed to better understand plaque morphology and was not powered to establish a link to clinical events.
Commenting for TCTMD, Ziad Ali, MD (NewYork-Presbyterian/Columbia University Irving Medical Center, New York, NY), said that conclusion is appropriately cautious considering the fact that OCT was not performed in the nonculprit lesions of patients randomized to culprit-only PCI in the trial.
“What this study does is it points us in the direction that in those patients that underwent complete revascularization, the nonculprit arteries showed a high proportion of thin-cap fibroatheroma and a high proportion of lipid, and what that does is it [suggests] that nonculprit lesions in a STEMI population may be a particularly high-risk group,” Ali said. He explained that OCT results would be needed in the culprit-only arm of the trial in order to make the connection between the reduction in clinical events seen with complete revascularization and stenting of vulnerable plaques in nonculprit lesions.
“What’s left for us to extrapolate is the idea that in the incomplete group, those were actually the lesions that led to myocardial infarction. That’s the missing link,” he said.
COMPLETE OCT Substudy
The COMPLETE trial showed that complete revascularization reduced risks of CV death or new MI (HR 0.74; 95% CI 0.60-0.91) and CV death, new MI, or ischemia driven revascularization (HR 0.51; 95% CI 0.43-0.61) compared with culprit-only PCI.
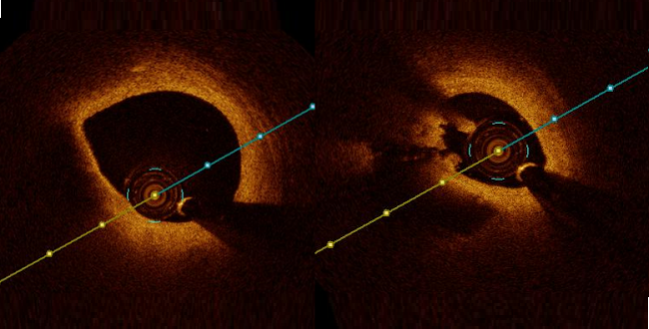
Whether the benefits seen with stenting obstructive nonculprit lesions is related to underlying vulnerable plaque morphology is unclear, Pinilla-Echeverri said. She explained that OCT can identify vulnerable plaques like TCFAs, which have been shown to be precursors of plaque rupture and powerful predictors of subsequent CV events.
In this substudy, the investigators examined plaque morphology with multivessel OCT in 93 patients (mean age 61.2 years; 83% men) who were randomized to complete revascularization in the larger COMPLETE trial. Imaging was performed in the vessel containing the obstructive nonculprit lesion slated for PCI, an additional vessel with or without a target nonculprit lesion for PCI, and the culprit vessel if there was at least 50 mm of unstented segment.
Overall, there were 425 nonculprit lesions evaluated; 31% contained a TCFA. The fact that so many lesions were found in only 93 patients “is reassuring that the concept of acute coronary syndrome implies a diffuse pathophysiology affecting not only the culprit segment but the coronary vasculature as a whole,” Pinilla-Echeverri said.
As hypothesized, the prevalence of TCFA was higher in obstructive versus nonobstructive nonculprit lesions (35.4% vs 23.2%). In addition, obstructive TCFA lesions were longer and had a small minimum lumen area compared with nonobstructive TCFA lesions.
When looking only at obstructive lesions, those containing TCFAs had significantly greater lipid infiltration, lower mean fibrous cap thickness, and greater degrees of macrophages and cholesterol crystals compared with those without TCFAs, which were mostly fibrotic and calcified, Pinilla-Echeverri reported.
Nearly half of patients had an obstructive nonculprit lesion containing a TCFA, 20.4% had a TCFA only in a nonobstructive nonculprit lesion, and the remaining 32.3% did not have vulnerable plaque identified.
“This study, in the context of a large, well-powered randomized controlled trial [that] showed a clinical outcome [benefit], provides further support for the concept of the vulnerable plaque in the vulnerable patient,” Ali commented.
Important Pathophysiological Information
Serving as a discussant for the study, Frans Van de Werf, MD, PhD (KU Leuven, Belgium), said the fact that nearly half of patients with STEMI and obstructive multivessel disease were shown to have nonculprit lesions with vulnerable plaque morphology “immediately explains the benefit of preventive PCI” that has been seen in COMPLETE and other trials.
Another finding of interest is that about one-fifth of these patients had vulnerable plaques in nonobstructive lesions only. “And of course, this finding . . . supports the immediate start of intensive lipid-lowering therapy, mainly with statins, as recommended by guidelines,” Van de Werf said.
As for the remaining patients who had obstructive nonculprit lesions without vulnerable plaques, the best treatment strategy is unclear, he said.
He said additional questions revolve around how and when the identify and treat lesions that are suitable for revascularization, as the recent trials comparing complete and culprit-only PCI have differed in these respects and, in particular, in use of OCT or fractional flow reserve (FFR).
“This OCT substudy provides, I think, important pathophysiological information for further treatment post-PCI in STEMI patients with nonculprit obstructive lesions,” Van de Werf said. “I believe that OCT and FFR should not be performed during index primary PCI, not only for the comfort of the patient but also for the better selection of the complete revascularization of the patient.”
He urged interventional cardiologists to not forget that CABG might be a better revascularization option than PCI for nonculprit lesions in some cases.
“I believe that if the choice of revascularization—PCI or CABG—of nonculprit lesions is made during the index PCI in the acute phase, CABG is less likely to be chosen,” he said, pointing to data from the STREAM 1 study to support his stance.
Photo Credit: Park S-J. Treatment of vulnerable patients and plaques: PREVENT rationale and update. Presented at: TCT 2019. September 27, 2019. San Francisco, CA.
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Pinilla-Echeverri N. Non-culprit lesion plaque morphology in patients with ST-segment elevation myocardial infarction: results from the COMPLETE trial optical coherence tomography (OCT) substudy. Presented at: AHA 2019. November 17, 2019. Philadelphia, PA.
Disclosures
- The COMPLETE OCT substudy was supported by Abbott Vascular, the Population Health Research Institute, Hamilton Health Sciences, and the Canadian Institutes of Health Research.
- Pinilla-Echeverri reports serving as a speaker for Abbott and receiving honoraria from Conavi.
- Van de Werf reports no relevant conflicts of interest.


Comments