CRT Patients Fare Better With LBB Area vs Biventricular Pacing
Despite the positive results, there are open questions about LBB pacing, including long-term lead performance. RCTs are coming.
SAN DIEGO, CA—Left bundle branch area pacing (LBBAP) is associated with better outcomes than biventricular (BiV) pacing among patients with an LVEF of 50% or less requiring cardiac resynchronization therapy (CRT), according to results from the International Collaborative LBBAP Study (I-CLAS).
Patients treated with LBBAP had lower rates of adverse clinical outcomes and arrhythmic events along with greater improvements in LVEF, Pugazhendhi Vijayaraman, MD (Geisinger Heart Institute, Wilkes-Barre, PA), reported recently at Heart Rhythm 2025.
The current analysis is based on previously published comparisons of the two pacing types in separate cohorts of patients with LVEF 35% or less and 36% to 50%, with strict propensity- score matching to account for baseline differences.
“Conduction-system pacing, especially the left bundle branch area pacing, has been shown to be a safe, physiologic, and effective alternative to biventricular pacing,” Vijayaraman said.
While CRT with BiV pacing is an established therapy in patients with reduced LVEF, heart failure, wide QRS, and need for frequent ventricular pacing, conduction-system pacing, either at the His-bundle or LBB, has emerged as an alternative. Recommendations from the European Society of Cardiology, European Heart Rhythm Association, and Heart Rhythm Society all say there is a role for conduction-system pacing in practice.
The International Collaborative LBBAP Study
I-CLAS is a nonrandomized, retrospective, observational cohort study that includes patients undergoing successful CRT with either LBBAP or BiV pacing. The new analysis included 2,579 patients (mean age 70 years; 32% women) who had an LVEF of 50% or less, NYHA class II-IV heart failure (HF) symptoms, a QRS duration of 130 ms or greater or more than 40% anticipated ventricular pacing, and follow-up of at least 6 months.
At baseline, the two pacing groups differed in age, sex, hypertension, type of cardiomyopathy, and ejection fraction. Propensity-score matching left 780 well-balanced pairs of patients (mean age 70 years; 34% women). Two-thirds had nonischemic cardiomyopathy, with a mean ejection fraction of 29%. Mean baseline QRS duration was 159 ms, and 54% had left bundle branch block. Most (70%) had a primary CRT indication.
BiV pacing was associated with more procedural complications overall versus LBBAP (6.5% vs 3.5%; P = 0.004). Those included pericardial effusion (1.2% vs 0.5%), pneumothorax (0.3% in each), acute lead dislodgement (2.9% vs 1.2%), infection (2.4% vs 1.2%), acute perforation of the left ventricle (0 vs 0.1%), and hematoma requiring intervention (0.1% vs 0.2%).
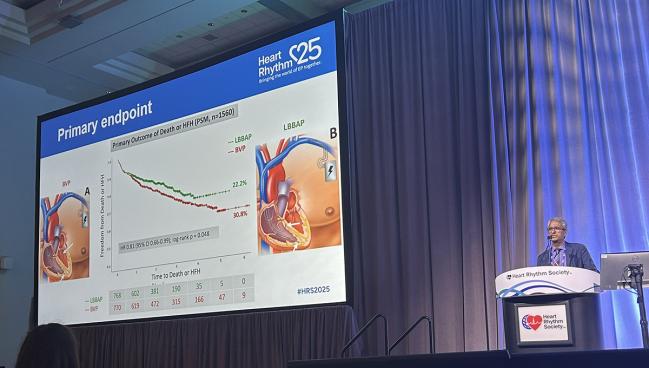
Differences between groups in adverse clinical outcomes emerged in up to 5 years of follow-up. The primary outcome was a composite of death or a first HF hospitalization, and this occurred less frequently with LBBAP than with BiV pacing (22.2% vs 30.8%; HR 0.81; 95% CI 0.66-0.99).
The difference was driven by a significantly lower rate of HF hospitalization (13.6% vs 20.8%; HR 0.63; 95% CI 0.49-0.82), without a significant difference in all-cause mortality (12.4% vs 18.2%; HR 0.82; 95% CI 0.63-1.07).
Conduction-system pacing, especially the left bundle branch area pacing, has been shown to be a safe, physiologic, and effective alternative to biventricular pacing. Pugazhendhi Vijayaraman
LBBAP also was associated with a greater improvement in LVEF—by about 12% versus 9% (P < 0.001)—and a greater likelihood of having gains of at least 5% (about 67% vs 59%; P < 0.001) or 15% (about 36% vs 28%; P = 0.004).
Arrhythmic events occurred less frequently with LBBAP as well:
- Nonsustained ventricular tachycardia (4.9% vs 10.9%; P < 0.001)
- Sustained ventricular tachycardia/fibrillation (4.0% vs 8.1%; P < 0.001)
- Implantable cardioverter-defibrillator shocks (3.7% vs 6.8%; P = 0.006)
- New-onset atrial fibrillation (2.3% vs 8.5%; P < 0.001)
Vijayaraman acknowledged that the study was limited by its retrospective, observational design, which is open to possible selection and population biases; the use of an on-treatment but not intention-to-treat analysis; and the involvement of centers with extensive experience in LBBAP, raising questions about how the results would apply at less-experienced sites.
Randomized Data Needed
Rajesh Kabra, MD (Kansas City Heart Rhythm Institute, Overland Park, KS), the discussant for the trial, pointed to those and other limitations, including disparities between the LBBAP and BiV groups at baseline.
Although the findings suggest a difference between pacing types, “the clinical outcomes of BiV pacing versus left bundle branch area pacing need to be studied in large prospective randomized clinical studies, some of which are ongoing and will be crucial to establish the superiority of conduction-system pacing,” Kabra said.
He added that there are needs for longer-term data to assess the performance of LBBAP leads and their extractability; improvements in implantation techniques and tools to achieve better LBBAP lead placement; and device algorithms tailored for conduction-system pacing.
“For now, an individualized approach to CRT implant strategy with BiV or left bundle branch area pacing according to patients’ characteristics and operator experience needs to be undertaken to achieve good clinical outcomes,” Kabra said.
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Vijayaraman P. LBBAP compared to BVP in candidates for cardiac resynchronization therapy (LVEF ≤50%): results from International Collaborative LBBAP Study (I-CLAS). Presented at: HRS 2025. April 25, 2025. San Diego, CA.
Disclosures
- Vijayaraman reports consulting for and receiving research and fellowship support and honoraria from Medtronic; consulting for and receiving honoraria from Boston Scientific and Biotronik; consulting for and receiving research support from Abbott; and holding a patent for a His-bundle pacing delivery tool.
- Kabra reports no relevant conflicts of interest.





Comments