DESolve Bioresorbable Stent Compares Well With Absorb, but Longer Follow-up Needed
Data beyond 1 year are required to better understand the relative safety and efficacy of these two bioresorbable scaffolds.
A matched comparison of two disappearing stents, one of which dissolves as early as 1 to 2 years after implantation, suggests the two platforms perform equally well and result in similar clinical outcomes.
The study, which included patients treated with the Absorb everolimus-eluting bioresorbable vascular scaffold (BVS, Abbott Vascular) and the DESolve novolimus-eluting scaffold (Elixir Medical), showed no statistically significant difference in the 1-year rate of target lesion failure between the two stent arms (4.7% vs 4.5%, respectively; P = 0.851).
Overall, just five stent thrombosis events were reported, with investigators stating there was no significant difference between those who received the Absorb and DESolve stents (2.0% vs 1.0%, respectively; P = 0.529).
“The present study reveals that implantation of [Absorb] or [DESolve] in routine clinical practice is effective in general and is associated with reasonable clinical outcomes in a large variety of patients and anatomical settings,” lead investigator Jens Wiebe, MD (University of Giessen, Germany), and colleagues write in their paper published February 15, 2017, in JACC: Cardiovascular Interventions.
The researchers add that the difference in the stent design and drug elution did not affect other parameters, such as procedure time, radiation time, or the amount of contrast agent used.
European Insights
Both bioresorbable stents are commercially available in Europe, although Absorb, which begins to degrade after 12 months and is fully dissolved between 2 and 3 years, has cornered the largest proportion of the European market. In the United States, only the Absorb BVS is available, with the US Food and Drug Administration approving that stent for use in 2016. As reported by TCTMD, a number of companies are currently testing a variety of bioresorbable stent technologies in clinical trials. Each of these devices is designed a little differently, with varying strut thickness, drug-elution profiles, and rates of degradation.
To TCTMD, Wiebe noted that the DESolve stent is also “self-correcting,” which allows the device to expand under nominal pressure in the case of an underexpanded stent. Also, bench testing suggests the fracturing threshold is lower with DESolve than with Absorb; this allows operators to give greater pressure after implantation.
Speaking with TCTMD, Davide Capodanno, MD (University of Catania, Italy), said the single-center matched comparison of ABSORB and DESolve is interesting as most clinical centers don’t have access to both stent technologies. Moreover, companies have little financial incentive to conduct a head-to-head comparison of the bioresorbable scaffolds. At his high-volume institution, only about 6% of patients receive Absorb BVS and they do not stock the novolimus-eluting scaffold.
Capodanno, who wrote an editorial accompanying the study, noted that both Absorb BVS and DESolve are first-generation bioresorbable scaffolds with some design similarities. Both stents are made of poly-L-lactide (PLLA), and they have approximately the same crossing profile and strut thickness (150 µm). And while there are some design differences, including differences in radial strength (DESolve is stronger), the impact of the different resorption rate between stents will require longer-term follow-up, he said.
“What will be more interesting are the results after 1 year because one of the stents (DESolve) is going to disappear and the other is going to stay,” said Capodanno. “In the future, it will be important to understand if the resorption time is something that should be shorter or longer. One might also question if there is too short [a time] in the coronary vessel then there’s less scaffolding function. It’s a trade-off between the good and bad of a stent being in there.”
Matching Patients and Procedural Variables
In the German single-center study, investigators studied consecutive patients treated with either bioresorbable scaffold. In total, 212 patients who received Absorb BVS and 106 patients who received DESolve were included in the propensity-matched analysis. In addition to being matched for baseline patient characteristics, the researchers matched patients based on two procedure-related factors—predilatation and postdilatation, both of which are considered necessary to optimize PCI outcomes with bioresorbable stents.
It’s a trade-off between the good and bad of a stent being in there. Davide Capodanno
Overall, approximately 50% of patients were treated for ACS in both arms and a little less than half had complex lesions. The average lesion length was a little more than 12 mm. Intravascular imaging was used in 36% of cases with Absorb BVS and 52% of DESolve cases.
At 1 year, the rate of major adverse cardiovascular events was 5.8% with Absorb and 4.5% with DESolve, a nonsignificant difference. Regarding individual components of the device-related target lesion failure endpoint, there was no differences between the two stents. Subacute scaffold thrombosis occurred in two patients treated with Absorb (day 4 and day 17) and in one patient treated with DESolve. Two late scaffold thromboses occurred in the Absorb arm, one at day 38 and the other at day 77.
“We found no relevant differences in terms of outcomes, including myocardial infarction and target lesion revascularization and maybe the most important endpoint, scaffold thrombosis,” said Wiebe. “We didn’t find differences in the matched population or in the unmatched population.”
To TCTMD, Capodanno said that given the similarities of the two stents, including strut thickness, it’s unlikely clinical events would differ between Absorb and DESolve at such an early time point. Should any meaningful differences emerge between them, specifically with regard to late scaffold thrombosis, follow-up of 5 years would be needed, he added.
To date, however, long-term clinical outcomes are limited with the bioresorbable scaffolds, and those that are available, specifically the 3-year clinical outcomes from ABSORB II, have underwhelmed. In October 2016, as reported by TCTMD, investigators reported that treatment with Absorb BVS did not result in an improvement in vasomotor tone and was associated with an increase in late lumen loss compared with the Xience everolimus-eluting metallic stent (Abbott Vascular). The rate of target-vessel MI was also higher with Absorb.
Regarding the rate of target lesion failure in the single-center study, Capodanno said it’s within the “acceptable range,” although he pointed out the study was not randomized and subject to selection bias. The 1-year rate of target lesion failure with the Absorb BVS was 7.8% in the ABSORB III trial, he noted.
Longer-term follow-up with the DESolve stent is available, with 4-year data from the first-in-human DESolve Nx study presented at TCT last year. In that study, there was no catch-up of late clinical events observed between 1 and 4 years, said Capodanno. That study, however, was very small with just 122 patients, he added.
In their paper, Wiebe and colleagues agree about the need for long-term follow-up and a larger study. Given its limitations, they say, the results of the present study should be considered “hypothesis generating.” They plan to follow their patients in this matched analysis for at least 3 years, Wiebe told TCTMD.
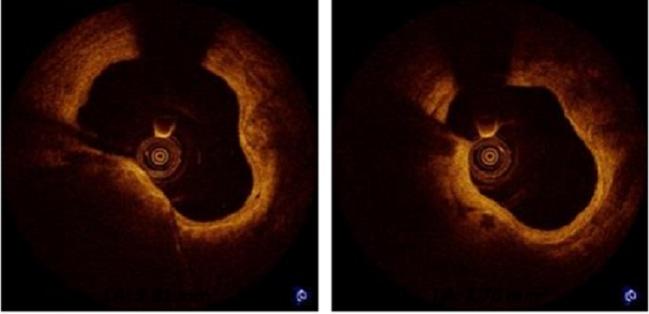
Photo Credit: Alexandre Abizaid, TCT 2016: Prospective, Multi-Center Evaluation of the DESolve Novolimus-Eluting Bioresorbable Coronary Scaffold: Imaging Outcomes and Four-Year Clinical and Imaging Results
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Wiebe J, Dörr O, Illstad H, et al. Everolimus- versus novolimus-eluting bioresorbable scaffolds for the treatment of coronary artery disease: a matched comparison. J Am Coll Cardiol Intv. 2017;Epub ahead of print.
Capodanno D. No apparent benefit of different drug or design on clinical outcomes of first-generation polymeric scaffolds: does resorption time play a better role? J Am Coll Cardiol Intv. 2017;Epub ahead of print.
Disclosures
- Wiebe reports no conflicts of interest. Disclosures for other authors are available in the paper.
- Capodanno is a consultant to Abbott Vascular.


Comments