Endothelial Dysfunction Observed Following Transradial Catheterization, Meta-analysis Suggests
Radial experts, however, argue that endothelial dysfunction is transient and the benefits of transradial access outweigh these small risks.
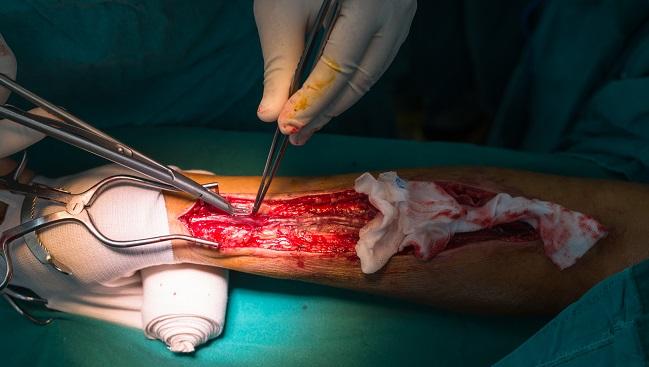
Using the radial artery for coronary angiography and interventional procedures impairs endothelial function for several months after the procedure, and this may contribute to reduced patency rates of catheterized radial arteries, according to the results of a new meta-analysis.
The researchers, led by Alexios Antonopoulos, MD (University of Athens Medical School, Greece), caution interventional cardiologists to use care when accessing the radial artery during coronary procedures, particularly in patients who may be eligible for radial artery grafts when CABG surgery is indicated.
Given that the radial artery is increasingly used as the access route of choice for coronary angiography, “the temporal change in interventional cardiology clinical practice is important since the radial artery is the second most common arterial graft next to the internal mammary artery in patients undergoing coronary artery bypass grafting,” according to the researchers.
Rodrigo Bagur, MD (Western University/University Hospital London Health Sciences Center, Canada), who was not involved in the study, told TCTMD that concerns about damage to the radial artery are unjustified.
“The most common radial site is the right radial approach, but the most commonly used radial conduit for coronary artery bypass grafting is the left radial artery,” said Bagur. “Additionally, the percentage of arterial revascularization which includes a [left internal mammary artery] graft to the LAD, a [right internal mammary artery] graft to another vessel, and the radial artery to a third vessel is very small. In current practice, it’s less than 20% of cases.”
He agreed there is a biological rationale for endothelial dysfunction following a puncture and cannulation of the radial artery, but such hypothetical risks need to be put in perspective given the reduced risk of bleeding and vascular complications, as well as the reduced risk of death, compared with transfemoral catheterization.
Unlikely to Impact Clinical Practice, Say Radial Operators
The study, which was published recently in the Journal of Cardiac Surgery, is based on an analysis of 12 studies that reported endothelium-dependent and independent vasodilatory responses of the radial artery following catheterization. The mean follow-up time was 3.8 months.
Overall, the researchers observed significant reductions in the endothelial-dependent response among treated patients (standardized mean difference -0.53; 95% CI -0.93 to -0.13), but only a marginal, nonsignificant reduction in endothelium-independent vasomotor function. In four studies that used the contralateral radial artery as a control, there was significant impairment in endothelial function more than 1 month after catheterization. The researchers observed significant heterogeneity among the analyzed studies.
In a marked regression analysis to identify predictors of endothelial dysfunction, they report that men had less radial artery dysfunction than women, possibly due to larger vessels and less mechanical injury. Additionally, increasing elapsed time after catheterization was predictive of less endothelial dysfunction, “suggesting the initial inflicted mechanical injury of the vascular endothelium is healed over time,” according to the researchers.
Bagur, who performs 99% of his cases via the radial artery despite working in a hospital that also performs a large number of CABG surgeries, said endothelial dysfunction is typically transient, often less than 30 days. “Therefore, in the case of patients who need left radial access for cardiac catheterization, and if it’s a clinically stable scenario, then the patient can undergo coronary artery bypass graft surgery after 30 days, which is always the case in stable patients,” he said.
The bottom line, said Bagur, is that these data should not discourage operators from transradial PCI given its proven advantages. “The benefits [compared with] transfemoral access have been demonstrated in a broad spectrum of patients,” he said.
Sanjit Jolly, MD (McMaster University, Hamilton, Canada), told TCTMD that cannulation of the radial artery is likely to have an impact on the vessel and that the right radial artery should not be used as a conduit if possible. “Practically speaking it is often not an issue, as interventionalists’ tend to use right radial and surgeons often use left radial,” he said via email. “However, if there are few conduits then this may become an issue . . . . Given the benefits of transradial interventions, I don’t think this is a valid reason not to use radial access.”
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Antonopoulos AS, Latsios G, Oikonomou E, et al. Long-term endothelial dysfunction after trans-radial catheterization: a meta-analytic approach. J Card Surg. 2017;32:464-473.
Disclosures
- Antonopoulos, Bagur, and Jolly report no relevant conflicts of interest.


Comments