Evolocumab Cuts MACE Risk in Patients Without Prior MI, Stroke: VESALIUS-CV
It’s the first study to show a PCSK9 inhibitor can reduce major events in high-risk patients who haven’t yet had one.
NEW ORLEANS, LA—A PCSK9 inhibitor used on top of lipid-lowering therapy, including a high-intensity statin, significantly cuts the risk of major adverse cardiovascular events compared with placebo when used in patients without a prior history of myocardial infarction or stroke, the VESALIUS-CV study shows.
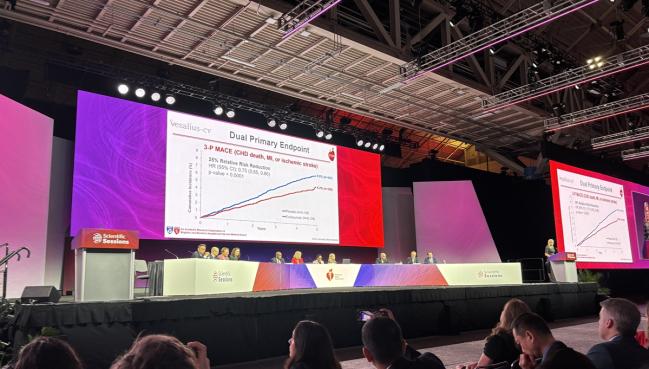
Over a median follow-up of 4.6 years, evolocumab (Repatha; Amgen) reduced the absolute risk of death from coronary heart disease, MI, or stroke by 1.8% (HR 0.75; 95% CI 0.65-0.86). When the primary endpoint was expanded to include ischemia-driven revascularization, evolocumab reduced the absolute risk by 2.8% compared with placebo (HR 0.81; 95% CI 0.73-0.89).
Lead investigator Erin Bohula, MD (Brigham and Women’s Hospital, Boston, MA), who presented the late-breaking trial at the American Heart Association 2025 Scientific Sessions, said treatment with evolocumab reduced LDL-cholesterol levels by a relative 55%, down to about 45 mg/dL.
“The VESALIUS-CV results support intensive LDL cholesterol-lowering, and one could argue maybe to a range of around 40 mg/dL, even in patients without a prior event,” she said during a media briefing. “I highlight that number because the most recent guidelines for extreme-risk patients, which is not this population, suggest going below a target of 40 mg/dL.”
While patients did not have a prior MI or stroke, researchers emphasized that the VESALIUS-CV participants still were at heightened risk for cardiovascular events: 67% had evidence of coronary heart disease, carotid artery disease, or peripheral artery disease and 33% had high-risk type 2 diabetes.
“In terms of identifying these patients, we see them a lot in clinic,” Bohula told TCTMD. “It’s that patient, for example, who has had a coronary revascularization but hasn’t had an MI that’s in this study. It’s a patient who has had long-standing diabetes, but you’ve done some evaluation and they don’t clearly have vascular disease, but you know they’re at risk: they’re older, maybe they’re on insulin, or they may have some degree of microvascular disease like renal dysfunction.”
The VESALIUS-CV results support intensive LDL cholesterol-lowering, and one could argue maybe to a range of around 40 mg/dL. Erin Bohula
Steven Nissen, MD (Cleveland Clinic, OH), who wasn’t involved in the study, called VESALIUS-CV a “good result” for physicians who care for these patients. “In this population, we lower LDL aggressively,” he told TCTMD. “I see these people all the time, and I throw the book at them to get their LDL levels down below 50 mg/dL.”
VESALIUS-CV is in line with prior studies showing that primary prevention patients at higher risk benefit from aggressive lipid-lowering therapy, said preventive cardiologist Kent Brummel, MD (University of Michigan, Ann Arbor).
“I think this will help support the expanded FDA indication for [evolocumab], which the FDA has granted for primary prevention,” he told TCTMD. “I think this will make it more accessible for patients and it gives us a little bit more of a foot to stand on for [primary prevention], although we already had reasonable evidence from other trials suggesting that you’d see this type of benefit if you expanded the use of PCSK9 inhibitors to other populations.”
In August, evolocumab was approved in high-risk adults without established disease to reduce the risk of major cardiovascular events (cardiovascular mortality, MI, stroke, unstable angina requiring hospitalization, or coronary revascularization). The approval took some by surprise, including Bohula and Brummel, who both said they thought the US Food and Drug Administration would wait until the results of VESALIUS-CV were published.
Amit Khera, MD (UT Southwestern Medical Center, Dallas, TX), who commented on the trial during the media briefing, said that even though the FDA approval for primary prevention came through, physicians were unlikely to use evolocumab in those without established cardiovascular disease given the lack of data. VESALIUS-CV help fills that gap, he said.
The VESALIUS-CV Trial
Evolocumab is approved for use in adults with established atherosclerotic cardiovascular disease (ASCVD) based on positive results from the FOURIER randomized trial. Alirocumab (Praluent; Regeneron/Sanofi) is also approved for secondary prevention based on the ODYSSEY Outcomes study.
VESALIUS-CV, which was published today in the New England Journal of Medicine, included 12,257 patients (mean age 66 years; 43% female) at high cardiovascular risk—defined as having diabetes plus a cardiovascular risk enhancer or atherosclerosis with or without diabetes and elevated LDL cholesterol (≥ 90 mg/dL)—randomized to placebo or evolocumab 140 mg every 2 weeks.
Two-thirds of patients had atherosclerosis, including 45% with coronary artery disease, 10% with cerebrovascular disease, and 17% with peripheral artery disease. Half of patients had diabetes, with 33% having a diagnosis of diabetes without atherosclerosis. More than 90% of patients were on lipid-lowering therapy and 72% were treated with high-intensity lipid-lowering therapy. In all, 87% were treated with a statin (68% on a high-intensity statin). The median baseline LDL-cholesterol level was 122 mg/dL.
I see these people all the time, and I throw the book at them. Steven Nissen
In addition to the 25% and 19% relative reductions in the three- and four-point MACE endpoints, respectively, evolocumab cut the risk of most secondary endpoints in hierarchical testing. Death from cardiovascular causes, MI, or ischemic stroke was reduced by an absolute 2.3% (HR 0.73; 95% CI 0.64-0.84). The absolute risk of MI was reduced by 1.4% (HR 0.64; 95% CI 0.52-0.79) and the risk of revascularization by 2.4% (HR 0.79; 95% CI 0.70-0.88).
There was no significant reduction in the risk of death from coronary heart disease or ischemic stroke alone, but both outcomes were numerically lower with evolocumab. Reductions in the risk of all-cause mortality and cardiovascular mortality went in the direction favoring evolocumab but should be considered hypothesis-generating based on hierarchical testing.
The benefit of treatment on both MACE endpoints was seen across all subgroups. There were no safety issues seen with evolocumab.
Identifying High-risk Patients
During the briefing, Khera pointed out that evolocumab was first approved as an agent to lower LDL cholesterol a little more than 10 years ago. Over the decade, much has been learned about the PCSK9 inhibitors, “but there’s some important questions that have remained, and I feel like this trial has answered them to a good degree,” he said.
First, the 25% relative reduction in VESALIUS-CV is notable because clinicians have suspected evolocumab’s benefit would be larger in a trial of longer duration. In FOURIER, for example, the relative reduction in MACE was just 15% compared with placebo during a median follow-up of 2.2 years. Second, the nominal reduction in all-cause mortality in VESALIUS-CV—7.9% in the evolocumab arm and 9.7% with placebo—is in line with the mortality benefit seen in ODYSSEY Outcomes, he said.
I think this will help support the expanded FDA indication for [evolocumab], which the FDA has granted for primary prevention. Kent Brummel
Khera noted that the treatment benefit was seen in patients with and without atherosclerosis. Among the 33% of patients with high-risk diabetes only, there was a 29% reduction in the three-point MACE endpoint with evolocumab, or a 2.1% absolute reduction compared with placebo. In those who qualified for the trial based on having atherosclerosis, evolocumab cut the relative risk of the three-point MACE endpoint by 24%.
Identifying higher-risk patients who have not yet had a first cardiovascular event is something that preventive cardiologists have been thinking about quite a bit lately, said Brummel. Patients with existing atherosclerosis are often found through incidental testing, he said.
“They go in for a CT scan or an ultrasound for another reason and it’s noted that they have coronary artery calcification or carotid artery plaque,” he said. “Using that as a way to identify patients who are at higher risk is growing. In most health systems, the radiologist will comment on coronary artery calcification, specifically, whenever that’s included within the field of view of the CT scan. That’s one way in which these patients can be identified when they are asymptomatic.”
The other way is with formalized coronary artery calcium testing, which is popular for patients who are at intermediate risk but undecided about starting statin therapy, said Brummel.
For VESALIUS-like patients, Brummel said that he would consider using a PCSK9 inhibitor based on their lipid profile alone. Although the large majority of patients were on statin therapy, including high-intensity statins, LDL cholesterol, non-HDL cholesterol, and apolipoprotein B levels were above the currently recommended targets (122, 153, and 100 mg/dL, respectively).
“Plus, they’re a higher-risk person based on the other comorbidities,” said Brummel. “In that context, I have already been offering PCSK9 inhibitors because I think the observational studies have suggested benefit. Now we have more evidence for that approach.”
Nissen agreed, saying that he would not leave such a high-risk patient with a median LDL-cholesterol level of 122 mg/dL. One minor criticism of VESALIUS-CV, he said, is that just 20% of patients were treated with ezetimibe. Insurance companies, he noted, want physicians to start with high-intensity statin therapy, followed by ezetimibe. If unable to get to goal with that combination, a PCSK9 inhibitor is the next option, he said.
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Bohula EA, Marston NA, Bhatia AK, et al. Evolocumab in patients without a previous myocardial infarction or stroke. N Engl J Med. 2025;Epub ahead of print.
Disclosures
- Bohula reports consulting for, receiving trial funding from, and/or having other relationships with Amgen, Anthos, AstraZeneca, Boehringer Ingelheim, CeleCor, Daiichi Sankyo, Esperion, Kowa, Merck, Novartis, Novo Nordisk, Pfizer, Regeneron, Roche, Entity, Servier, Siemens, Softcell, and Verve Therapeutics.





Comments