Experts Debate: Is It ‘Nuts’ to Restart Anticoagulation After Lobar ICH?
Restarting is like “a gun to the head,” says Stephan Mayer, while Alessandro Biffi argues that there’s a benefit in some patients.
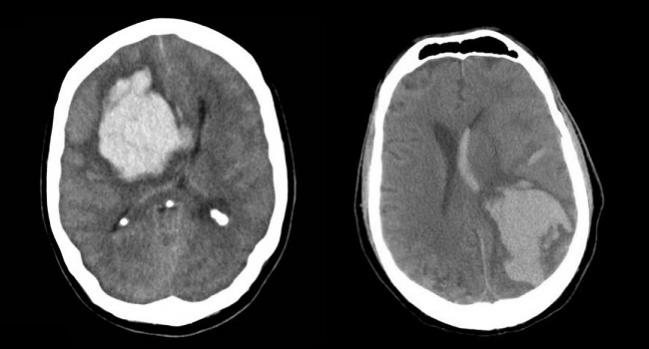
LOS ANGELES, CA—Here at the International Stroke Conference, two experts had a lively debate about whether it is advisable to put patients back on oral anticoagulation after they’ve had a lobar intracerebral hemorrhage (ICH).
Leading off, Stephan Mayer, MD (Henry Ford Health System, Detroit, MI), didn’t mince words: “Are you crazy? Somebody comes in with a lobar intracerebral hemorrhage, probably from amyloid angiopathy, and you’re going to put them on blood thinners? I think that’s nuts.”
But Alessandro Biffi, MD (Massachusetts General Hospital, Boston, MA), disagreed with making such a blanket statement. “I’m here to argue that some lobar ICH patients will benefit from resumption of oral anticoagulation,” he said. “They will find it both safe and beneficial.”
For the record, guidelines from the American Heart Association/American Stroke Association for the management of spontaneous ICH state that “avoidance of long-term anticoagulation with warfarin as a treatment for nonvalvular atrial fibrillation is probably recommended after warfarin-associated spontaneous lobar ICH because of the relatively high risk of recurrence (Class IIa; Level of Evidence B).”
Use of non-vitamin K antagonist oral anticoagulants in this setting is uncertain, according to the guidance.
‘Basically Pointing a Gun to Your Patient’s Head’
Mayer framed the issue by describing a hypothetical 69-year-old man with a history of A-fib who is taking oral anticoagulation when he presents with a spontaneous lobar ICH. After dealing with the acute issue, what should clinicians do?
This is a classic dilemma, and there are two choices, Mayer said. Doctors can play it safe and not restart anticoagulation, which will increase the risk of ischemic stroke a bit while lowering the risk of ICH. Or they can put the patient back on anticoagulation, which will lower ischemic stroke risk slightly while leading to a much higher risk of ICH.
ICH is the deadliest form of stroke, with a mortality rate of 50% to 70%, Mayer noted, adding that lobar ICH in particular is even worse.
Discussing the dilemma over whether to restart anticoagulation, Mayer pointed to a decision analysis that determined that withholding anticoagulation in survivors of lobar ICH who have A-fib improved life expectancy by 1.9 quality-adjusted life-years. “That means if you give the anticoagulation to your patient with lobar hemorrhage, you’ve wiped out 2 years of life,” he said.
Balancing the risks of thromboembolism and recurrent hemorrhage also favors not restarting therapy, he argued. Acute ischemic stroke risk among untreated patients with nonvalvular A-fib is 2% to 5% per year, with that risk decreasing on oral anticoagulation. But on the other side, the risk of recurrent ICH among untreated patients with a lobar hemorrhage probably related to cerebral amyloid angiopathy—which is estimated to cause 70% of lobar ICH—is 10.4% per year, with that risk rising on oral anticoagulation.
So if anticoagulation is restarted, “you’re basically pointing a gun to your patient’s head,” said Mayer, who noted that there are now effective devices—left atrial appendage occluders—for reducing ischemic stroke risk without increasing ICH risk.
Resumption Will Benefit Some Patients
Biffi argued for a selective approach to restarting oral anticoagulation after a lobar ICH, pointing out that this is already occurring in practice. A meta-analysis showed that 38% of patients with any type of ICH resumed treatment, and a study by Biffi’s group demonstrated that 28% of patients with nonlobar ICH and 23% with lobar ICH restarted anticoagulation.
In the latter study, going back on anticoagulation was associated with lower risks of all-cause and ischemic stroke without a significant increase in the risk of recurrent ICH through 1 year in patients with either lobar or nonlobar ICH. Functional outcomes according to scores on the modified Rankin Scale were improved in patients who resumed treatment as well.
Biffi said MRI data will be able to select patients with lobar ICH who are most likely to benefit from restarting anticoagulation, citing evidence suggesting that the balance of risks and benefits could favor resumption in patients with a low burden of cerebral microbleeds, no or focal cortical superficial siderosis, and A-fib with a high embolic risk.
“It may not be appropriate to restart oral anticoagulation for all lobar ICH survivors that were on it before, but some of them are very likely to benefit from it,” Biffi said. Randomized trials are urgently needed in this area, he added.
Confounded Results
In his rebuttal, Mayer said that studies showing better outcomes in patients who restarted anticoagulation suffer from confounding by indication and selection bias, because physicians are choosing which patients are likely to have a low risk of recurrence and derive a benefit from the move.
The paper from Biffi’s group is no different, he said: “It doesn’t prove anything.”
But, Biffi countered, if the findings of those studies are the result of confounding by indication or selection bias, it indicates that doctors are able to identify which patients will benefit.
“I’ll be happy with settling our discussion on the fact that I don’t think a one-size-fits-all answer to the question is fair,” he said. “We should not have a blanket statement that no one should [be] restarted on oral anticoagulation after a lobar intracerebral hemorrhage, because the existence of confounding bias implies that it is possible to . . . identify a meaningful group of patients that can be helped.”
Before the debate, an audience poll revealed that 27% agreed anticoagulation should not be restarted after lobar ICH, 58% disagreed with that statement, and 16% were undecided. The debate moved some of the undecideds off the fence, with a postdebate poll revealing rates of 30%, 62%, and 8% for the respective answer choices.
Photos Credit: A.Prof Frank Gaillard, Radiopaedia.org, Case 1, Case 4.
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Mayer SA. Anticoagulation therapy should not be restarted in patients with anticoagulation-related lobar intracerebral hemorrhage (YES). Presented at: ISC 2018. January 26, 2018. Los Angeles, CA.
Biffi A. Anticoagulation therapy should not be restarted in patients with anticoagulation-related lobar intracerebral hemorrhage (NO). Presented at: ISC 2018. January 26, 2018. Los Angeles, CA.
Disclosures
- Mayer and Biffi report no relevant conflicts of interest.


Comments