Experts Fear Coronary CT Advice for Patients Misses the Mark
An article aimed at the lay public contains misinformation and errors, and it may mislead patients, prominent cardiologists say.
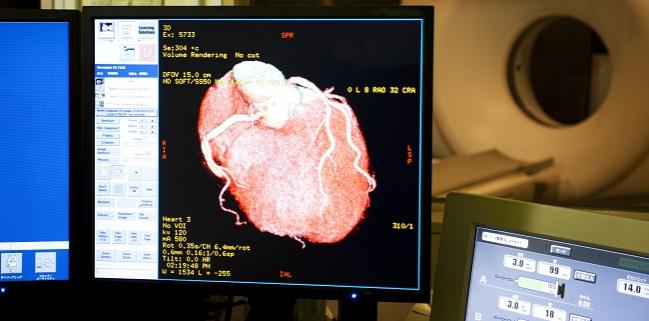
An article in JAMA Internal Medicine dedicated to informing patients of the pros and cons of coronary CT angiography is drawing criticism from cardiologists, including some involved in drafting guidelines for the prevention of cardiovascular disease and the treatment of high cholesterol.
On a “patient page,” Michael Incze, MD (University of Utah, Salt Lake City), outlines the potential benefits and harms of coronary CT, including CT angiography and coronary artery calcium (CAC) scans, warning that such scans can lead to increased worry, overtreatment and overtesting, exposure to radiation, and higher healthcare costs without providing specific information to help patients lower their chance of heart attacks. Incze also writes that existing risk calculators are better at estimating a patient’s risk than either of the coronary CT scans.
“Many community clinics advertise coronary artery calcium scans, also known as heart scans, to assess the risk of heart attack,” writes Incze. “There is no evidence that these scans provide any benefit, and they are of questionable quality.”
Some experts, however, are calling the article “misinformed.”
Donald Lloyd-Jones, MD (Northwestern University Feinberg School of Medicine, Chicago, IL), president-elect of the American Heart Association, kicked off the conversation on Twitter, saying the patient page “cites out of date and incorrect information, and completely misleads patients,” particularly when it comes to the utility of CAC scans. To TCTMD, Lloyd-Jones emphasized that while patient pages can be very helpful, it’s important the information is clear and accurate.
Unfortunately this piece in @JAMAInternalMed is misinformed, cites out of date and incorrect info, and completely misleads patients about the utility of CAC. It can be our most helpful prevention decision tool when used appropriately. Get the facts right!https://t.co/AYL6MS0cV9
— Don Lloyd-Jones (@dmljmd) March 16, 2021
“One of the major problems here is that they’re lumping calcium scoring and CT angiograms together,” he said. CT angiography is used as a niche noninvasive test in patients with chest pain symptoms, while CAC testing is used primarily as a decision tool for the primary prevention of heart disease. “We’re talking about two entirely different patient populations who might get these tests,” he continued, “yet it seems to me lumping them together creates a lot of confusion in terms of when you might need one or the other.”
For Lloyd-Jones, the bulk of the misinformation stems from how CAC testing is presented to patients. He acknowledges there are no randomized controlled trials using coronary calcium as a decision tool to improve clinical events, but said those studies, including ROBINSCA, DANCAVAS, and others, are ongoing. “In the meantime, I think there is a substantial amount of evidence from studies such as MESA, CARDIA, and others that show us definitively that we can make better decisions about who needs prevention using [CAC] appropriately,” said Lloyd-Jones. “Like most tests in medicine, it makes a difference who we use it in. I think we can all agree that we shouldn’t be doing routine screening of everybody in the population.”
A Time and Place for CAC
The 2018 American College of Cardiology/American Heart Association cholesterol guidelines recommend using CAC screening to help make decisions about patients who fall into the “gray zone” for treatment. Lloyd-Jones said the first step is to assess patient risk using the pooled cohort equations and then the next is to personalize that risk estimate by taking into account other variables, such as family history or the presence of chronic kidney disease. For the patients where it’s uncertain if a statin should be started, such as those at intermediate risk or even borderline risk, or if there is some hesitancy on the part of the patient, then CAC testing can help inform that decision.
“You can’t look at this test in isolation,” said Lloyd-Jones. “You have to look at in the context of the whole prevention conversation. The [patient page] doesn’t acknowledge this.”
In the article, Incze also writes that “established risk calculators are more effective at estimating the risk of heart attack,” but Lloyd-Jones says that’s flat-out wrong. Additionally, Incze contends that CAC scores are not modified by lifestyle or medication, but Lloyd-Jones says this again is off the mark. Coronary calcium is not plaque—it’s tightly correlated with the overall burden of plaque—and it’s not expected to change as a result of interventions. The interventions, such as lifestyle and medication, are instead expected to be more beneficial in these patients because they have a greater plaque burden.
“We’re not looking to remove the calcium,” said Lloyd-Jones. “One, you can’t, and two, calcium is there as a stabilizing agent in the plaque. This is fundamental misunderstanding of why we look for CAC and what it represents.”
Like most tests in medicine, it makes a difference who we use it in. I think we can all agree that we shouldn’t be doing routine screening of everybody in the population. Donald Lloyd-Jones
Michael Blaha, MD (Johns Hopkins Ciccarone Center for the Prevention of Heart Disease, Baltimore, MD), also commenting for TCTMD, said JAMA Internal Medicine is a highly prestigious journal from the American Medical Association. Yet, he added, this patient page fails to reference the multiple clinical guidelines, including those from the US, Europe, and beyond, that have endorsed CAC as a clinical decision aid. He’s concerned that patients will read the page, specifically the statement that “neither [CT angiography nor CAC] is a proven tool for estimating the risk of heart attack,” and come to the conclusion that CAC is just one of many tests developed over the years that don’t work.
Calcium scoring absolutely does predict the risks of future clinical events, and does so on top of conventional risk factors, said Blaha.
TCTMD reached out to Rita Redberg, MD (University of California, San Francisco), the editor of JAMA Internal Medicine, to ask about these criticisms, as well as the online debate, but a spokesperson for the journal said they had no comment on the patient page.
Benefit vs Harm
As for the harms associated with CAC scoring, Lloyd-Jones said radiation exposure is low, equivalent to mammography. With respect to downstream testing, the EISNER trial showed that patients undergoing CAC testing had better risk factor control and were unlikely to undergo further testing or invasive procedures if the CAC scores were low. To TCTMD, Blaha said the National Lipid Association (NLA), which earlier this year endorsed the use of CAC as a decision aid for preventive therapies in selected patients, recommends against any downstream testing in asymptomatic patients after CAC screening (class III).
“This is the strongest statement on the topic to date,” said Blaha, referring to the NLA guidelines that he co-authored. “It shows how far the field has come, and it is why concerns about downstream testing, cost, caths, and stents are mostly out of date.”
The United States Preventive Services Task Force (USPSTF) published a review in 2018 stating the current evidence is insufficient to assess the balance in benefits and risks of CAC screening, or other nontraditional risk factors, when added to traditional risk assessment tools for preventing cardiovascular events in asymptomatic adults. However, the outcome trials are coming, said Lloyd-Jones. In the meantime, he considers CAC screening a low-risk tool that can help physicians make better decisions when used in a selected way the guidelines recommend.
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Incze MA. Should I get a coronary CT scan? JAMA Intern Med. 2021;Epub ahead of print.
Disclosures
- Incze, Lloyd-Jones, and Blaha report no conflicts of interest.



Comments