Plaque Burden, Not Coronary Stenosis, Linked to Future Events in Stable CAD
Taking a broad view of atherosclerotic burden allows physicians to focus on stable patients at highest risk for future CVD.
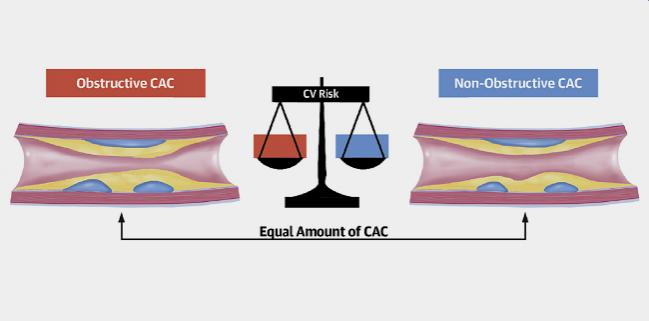
Increasing plaque burden based on the coronary artery calcium (CAC) score and the presence of obstructive coronary artery disease on CT angiography are both associated with an increased risk of future cardiovascular events, but a new analysis suggests it’s the overall coronary plaque burden that appears to be the driving force behind patient risk.
For patients with equal burdens of coronary calcification, the presence and number of vessels with a stenosis ≥ 50% were not associated with higher future risk of MI, stroke, or all-cause mortality when compared with patients who have nonobstructive coronary disease, report investigators.
“We’ve known for many years that people who have stenosis on angiograms are high-risk patients and that is the reason we treat them,” said lead investigator Martin Bødtker Mortensen, MD, PhD (Aarhus University Hospital, Denmark). “The question is whether it’s the stenosis that puts them at risk or whether it’s because when you have a coronary stenosis you’re also more likely to extensive atherosclerotic cardiovascular disease.”
To TCTMD, Mortensen said the COURAGE, FAME, and ISCHEMIA trials have shown that while revascularization improves symptoms, there is no difference in hard clinical endpoints between patients with significant coronary stenosis who are treated with PCI/CABG surgery or guideline-directed medical therapy. That, he said, is an indication that it’s not the stenosis but rather the coronary artery disease burden that places these patients at a higher risk for CVD events.
“If you have the same degree of coronary calcium, which is a surrogate marker for atherosclerotic burden, it doesn’t matter if you have a stenosis or not,” said Mortensen. “You have the same degree of risk. I think these results are in line with the randomized trials [showing] that treating the stenosis is not that important. Instead, it’s treating the totality of atherosclerosis, and you can only do that with risk-factor control, such as lowering cholesterol, blood pressure, and so on.”
Don’t Focus Solely on Stenosis
Published online December 7, 2020, in the Journal of the American College of Cardiology, the analysis included 23,759 symptomatic patients (mean age 57.4 years; 44.6% women) from the Western Denmark Heart Registry who underwent diagnostic CT angiography. The overall population was relatively low risk, with just 13% reporting typical chest pain. Roughly half of patients did not have any traditional cardiovascular risk factors. Additionally, more than 50% of patients had a CAC score of zero.
Overall, the risk of major CVD events increased in a stepwise manner with increasing atherosclerotic disease burden by CAC and the number of vessels with obstructive disease. The event rate ranged from 6.2 to 42.3 per 1,000 person-years for patients with CAC scores of zero and > 1,000, respectively. Similarly, the event rate ranged from 6.1 to 34.7 per 1,000 person-years for patients with no obstructive CAD and patients with three-vessel obstructive CAD, respectively.
When researchers stratified patients into five categories based on CAC score (0, 1-99, > 100-399, > 400-1,000, and > 1,000), the risk of MI, stroke, and all-cause mortality was similar in patients with versus without obstructive CAD. For example, among those with a CAC score > 100-399, the event rates per 1,000 person-years were 17.9 and 17.3 in nonobstructive CAD and obstructive disease, respectively. Among patients with CAC scores > 400-1,000, the respective event rates per 1,000 person-years were 30.2 and 28.6 in those with nonobstructive and obstructive CAD.
“One of the most important messages of our study is that if you have a patient who has nonobstructive but extensive atherosclerotic disease, their risk of developing cardiovascular events afterwards is at least as high as those who have a coronary stenosis,” said Mortensen. “You have to treat them same way with intensive secondary medication.”
Mortensen said the new study suggests change is needed in the way physicians treat these symptomatic patients referred for angiography, either by CT or invasively, because the blockage is merely a symptom of diffuse atherosclerosis. “We’re really focused on the stenosis,” he said. “If they have a stenosis, they receive secondary prevention, but if they don’t, they tend to fall into the primary prevention category at least in many physicians’ minds. You have to stop that distinction between primary and secondary prevention when you do the CT scan, because it’s the burden of disease that matters.”
In an editorial, Todd Villines, MD, and Patricia Rodriguez Lozano, MD (University of Virginia, Charlottesville), say the emphasis on disease burden for a more complete evaluation of a patient’s risk “has never been more important” in light of ISCHEMIA showing that medical therapy should be the preferred approach in most patients with stable CAD. They both agree that it’s time traditional definitions of primary and secondary prevention change to include CAC and CT angiography measures of patient risk.
“The historical focus on lumen stenosis as the primary method for quantifying CAD severity and guiding prevention and interventional treatments in patients undergoing angiography must evolve,” they write. “Going forward, guidelines and the way clinicians discuss and address risk should incorporate the important prognostic data obtained from whole-heart atherosclerotic imaging provided by contrast and noncontrast cardiac CT. It should come as no surprise that for the prediction of atherosclerotic cardiovascular events, atherosclerotic plaque burden, regardless of stenosis, probably matters most.”
‘Power of Zero’ With CAC
Khurram Nasir, MD, MPH (Houston Methodist, TX), who wasn’t involved in the study, also said the new analysis reinforces the concept of disease burden as a more-important prognostic indicator than the conventional approach focused solely on coronary stenosis. “It’s also in line with what we have seen in the SCOT-HEART study,” he told TCTMD. “There, once you took into account the burden [of disease] with coronary calcium as a surrogate, the other features of the CT angiography didn’t really have any significant prognostic value.”
In addition, Mortensen et al provide yet more support for the “power of zero,” a concept that highlights the extremely favorable prognosis of individuals with a CAC of zero, said Nasir. In the present study, he noted that patients with a zero CAC score had a similar event as a patient with no CAD on CT angiography. “It adds to the ongoing and emerging evidence that has established a CAC score of zero to not only exclude obstructive disease, but adds another layer of reassurance,” he said. “An absence of calcium, a CAC of zero is as reassuring as if you’ve had a normal CT angiography.”
Nasir pointed to another study published just a few weeks back showing that the addition of the CAC score, along with cardiovascular risk factors, to the traditional diagnostic algorithm for chest pain could improve the prediction and discrimination of patients with CAD. In this way, CAC screening can serve as a gatekeeper and lower the pretest probability of disease in nearly two-thirds of patients who might be in line for advanced imaging, he said.
In the editorial, Villines and Lozano note that noncontrast CT for calcium scoring is not generally recommended as a stand-alone test for symptomatic patients. CT angiography, they say, has a higher diagnostic and prognostic accuracy than does CAC. In PROMISE, 16% of patients with a CAC score of zero had a CVD event, they add. Given these existing limitations, the most-recent European Society of Cardiology guidelines for chronic chest pain awarded CAC screening a class III recommendation for use in symptomatic patients, with CT angiography given a class I indication.
The long-awaited chest pain guidelines from the American College of Cardiology/American Heart Association are supposed to be released very shortly, and Nasir is hopeful there are enough data that CAC screening will be recognized as a gatekeeper for avoiding further downstream testing with a class IIa indication. “Of course, resources are not infinite, and thinking of this from a population standpoint and resource allocation, this might be a way where a calcium score of zero can reassure that the likelihood of having obstructive disease is very low and you can avoid further testing,” he said.
Photo Credit: J Am Coll Cardiol. Central Illustration (adapted).
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Mortensen MB, Dzaye O, Steffensen FH, et al. Impact of plaque burden versus stenosis on ischemic events in patients with coronary atherosclerosis. J Am Coll Cardiol. 2020;76:2803-2813.
Villines TC, Lozano PR. Transitioning from stenosis to plaque burden in the cardiac CT era: the changing risk paradigm. J Am Coll Cardiol. 2020;76:2814-2816.
Disclosures
- Mortensen, Villines, and Lozano report no relevant conflicts of interest.
- Nasir reports serving on advisory boards for Amgen, Novartis, and Esperion.


John Robert