EXPLANT-TAVR: Data Spur Conversation About Balancing Risk and Lifetime Management
The study is limited by lack of full procedural data, making it hard to interpret the high rates of endocarditis, says Sammy Elmariah.

Even in the hands of experienced heart teams, surgical explantation of TAVI valves continues to be associated with mortality risks that many patients may be unaware of and that need to be factored into decisions surrounding lifetime aortic stenosis management, according to a report from the EXPLANT-TAVR registry.
Endocarditis was a major reason for explantation in this series, the analysis found. Approximately one-third of patients could not undergo a redo TAVI, primarily due to unfavorable anatomy. Mortality was 13.1% at 30 days and 28.5% at 1 year.
“Most of these TAVR explant patients are high risk to start with and hence, they are going to have higher mortality,” said Vinayak N. Bapat, MD (Abbott Northwestern Hospital, Minneapolis, MN), lead investigator of the study, published in September 27, 2021, issue of JACC: Cardiovascular Interventions.
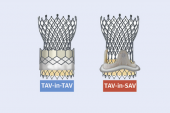
Even with a starting point of low risk, he said, more data are needed to understand which patients can be expected to do well with valve-in-valve TAVI, especially as more younger patients undergo TAVI and may outlive their devices. A problem that the registry data illustrate, Bapat added, is that the risks of explantation for some patients are higher than if they had initially undergone surgery.
In an accompanying editorial, Gorav Ailawadi, MD, and Karen M. Kim, MD (both University of Michigan, Ann Arbor), point out that the registry “lacks data on patients who had indications for TAVR explantation but were not surgical candidates and, importantly, for total volume of TAVR procedures performed across the centers during the study period to estimate the proportion of patients who required TAVR explantation.”
That last point also makes it difficult to know how to interpret the endocarditis data, said Sammy Elmariah, MD, MPH (Massachusetts General Hospital, Boston), who commented on the findings for TCTMD.
“If somebody remains a surgical candidate, explanting the infected valve is the preferred strategy. So, I'm not at all surprised by the frequency of seeing endocarditis being over 40% of the cases being explanted,” he said. “What we don’t know is the denominator, meaning we don't know how many TAVIs were performed in order to generate this number of explanted valves. So, this risk of endocarditis might be half a percent, or it could be one percent. We just simply have no idea.”
Concomitant Surgeries Elevate Mortality Risk
EXPLANT-TAVR included 269 patients from 42 centers in North America and Europe who underwent explantation procedures between 2009 and 2020. Of these, about 26% were considered low surgical risk at their index TAVI. Nearly 40% had a previous cardiac surgery and 70% had NYHA functional class III or IV symptoms. At the index TAVI, median STS risk score was 3.2%. At explantation, median STS risk score was 5.0%.
Explantation was due to endocarditis in 43% of cases, followed by structural valve degeneration in 20% and paravalvular leak in 18%. The rate of intraoperative mortality was 0.7%, while in-hospital mortality was 11.9%. About 16% of patients had life-threatening or major bleeding and 6% had permanent stroke.
The risk of endocarditis might be half a percent, or it could be one percent. We just simply have no idea. Sammy Elmariah
The median interval from index TAVI to explantation for the cohort was 11.5 months. More than one-third of the explant procedures occurred within 6 months, and half within 1 year. The majority of explanted patients (86.6%) received SAVR, 13.4% needed root replacement, and one-third of those with severe prosthesis-patient mismatch required both root replacement and root enlargement. Overall, about 55% of the cohort had a concomitant surgical procedure.
Looking at predictors of short- and long-term mortality, prior cerebrovascular disease, pulmonary hypertension, and concomitant mitral and/or tricuspid surgery during explantation were associated with increased 30-day mortality, while cardiopulmonary bypass time and concomitant mitral and/or tricuspid surgery were independent predictors of 1-year mortality.
A Need to Better Inform Patients
The registry also showed that patients who underwent TAVI explantation between 2017 and 2020 had worse early and 1-year mortality than those in the earlier part of the registry experience despite likely being a younger and lower-risk population, Ailawadi and Kim add. However, they say the EXPLANT-TAVR data are in line with reports from the Society of Thoracic Surgeons database and Medicare data, all three of which demonstrate high and similar mortality for explantation.
“When considering the lifetime management of patients with aortic valve disease, both TAVR and [surgical] AVR need to be discussed by the heart team,” they conclude. “Moreover, heart teams must recognize these data and inform patients about the risks associated with the need for TAVR explantation during the decision process.”
For Elmariah, the most valuable part of the EXPLANT-TAVR data is that they point to the challenges of performing TAVI for younger patients with the expectation that the device can be explanted down the road.
[Patients] may get the sense that TAVR explantation is not a big deal. Vinayak N. Bapat
“Explantation as a planned part of a patient's lifelong aortic stenosis strategy does not seem to make sense,” he observed. “I think it's something that should be reserved in those rare situations where you just simply have to take the valve out because of some unforeseen complication or change in the patient's clinical status.”
Another important point, he added, is that the need for concomitant mitral or tricuspid surgery should be mitigated as much as possible at the time of index TAVI.
“As we plan to treat patients using transcatheter means for their valvular heart disease, we need to ensure that we have an approach for each of the valve lesions. So, if the [mitral regurgitation], for example, was preexisting, then one very important thing to consider before proceeding with TAVI is to consider whether that patient's mitral valve disease can also be addressed using a transcatheter approach,” Elmariah said. “If it cannot be, then pushing that patient towards a surgical intervention instead of that initial TAVI would make sense.”
The problem, though, as both Elmariah and the EXPLANT-TAVR investigators note, is that it is unclear whether the valve lesions that required the concomitant surgeries were preexisting, or whether they developed or worsened in the years or months after TAVI.
Bapat said long-term results from PARTNER 3 and Evolut Low Risk will be impactful in terms of understanding the longevity of TAVI devices, which will likely improve decision-making and hopefully clarify issues of informed consent.
“I worry that we do not explain to patients what is really involved in the TAVR process, other than it’s a less-invasive therapy versus a more-invasive therapy, and so for them the choice is very obvious,” Bapat observed. “If they are a patient of 65, for example, they may think incorrectly that we can do [TAVR] over and over, or they may get the sense that TAVR explantation is not a big deal. As more choices become available, we need to [be able to] explain the long-term data to patients to help them decide. ”
L.A. McKeown is a Senior Medical Journalist for TCTMD, the Section Editor of CV Team Forum, and Senior Medical…
Read Full BioSources
Bapat VN, Zaid S, Fukuhara S, et al. Surgical explantation after TAVR failure: mid-term outcomes from the EXPLANT-TAVR international registry. J Am Coll Cardiol Intv. 2021;14:1978-1991.
Ailawadi G, Kim KM. Outcomes from the EXPLANT-TAVR registry: time to change TAVR informed consent? J Am Coll Cardiol Intv. 2021;14:1992-1994.
Disclosures
- Bapat reports serving as a consultant for Medtronic, Edwards Lifesciences, 4C Medical, and Boston Scientific.
- Ailawadi reports having served as a consultant for Abbott, Edwards Lifesciences, Medtronic, and Anteris.
- Kim reports no relevant conflicts of interest.
- Elmariah reports research grants from Edwards Lifesciences, Medtronic, and Abbott Vascular and consulting fees from Edwards Lifesciences.




Comments