FDA’s Proposed Sodium Reduction Plan Could Have a Big Impact, Analysis Suggests
Even in the most pessimistic scenario, the plan could prevent or postpone 120,000 CVD cases and save $12 billion over the next 20 years.
Full implementation of draft guidance from the US Food and Drug Administration (FDA) that establishes voluntary sodium reduction goals for commercially processed, packaged, and prepared foods could lower population blood pressure and stave off hundreds of thousands of cardiovascular disease cases and tens of thousands of related deaths over the next 20 years, a modeling study indicates.
If all 2- and 10-year reformulation targets are met (the “optimal” scenario), 450,000 CVD cases—with an uncertainty interval ranging from 240,000 to 740,000—and 35,000 related deaths could be prevented or postponed by 2036, according to a team led by Jonathan Pearson-Stuttard, BMBCh (University of Liverpool and Imperial College London, England).
That would be accompanied by a gain of about 2.1 million quality-adjusted life-years (QALYs) and a cost savings of about $41 billion after taking into account the costs incurred by food manufacturers to reformulate their products, they report in a study published online April 10, 2018, ahead of print in PLOS Medicine.
Even for the “pessimistic” scenario in which there is 100% compliance with the 2-year targets but no further improvements, 120,000 CVD cases would be avoided, 700,000 QALYs would be gained, and $12 billion would be saved over the next two decades. The “modest” scenario provides numbers falling between the other two.
Citing uncertainty in projecting out 20 years, Pearson-Stuttard told TCTMD that “we don’t get too fixated on the specific number. It’s the direction. All of these three scenarios consistently show—even when we’re taking into account all this uncertainty—that they would be very beneficial for the US population.”
Tackling Sodium at the Population Level
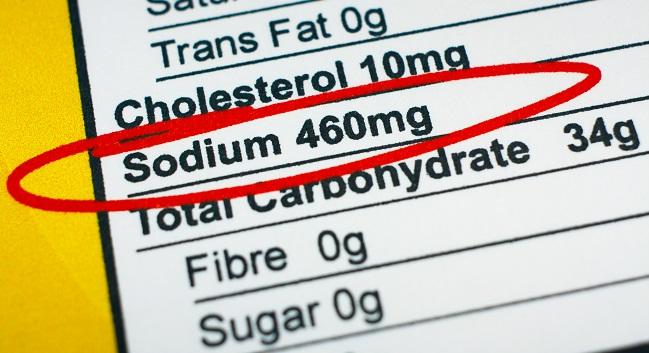
Average sodium intake in the United States is about 3,400 mg/day, much higher than the recommended upper level of 2,300 mg/day in the latest Dietary Guidelines for Americans. Most of that sodium—about three-quarters—comes from eating processed and commercially prepared foods, “making industry reformulation a major priority for reducing population sodium intake,” Pearson-Stuttard and colleagues write.
In line with that belief, in June 2016 the FDA released draft guidance detailing 2- and 10-year voluntary sodium reduction goals for makers of commercially processed, packaged, and prepared foods across 155 categories. The stated overall goal was to reduce sodium intake to 2,300 mg/day.
To estimate the health and economic effects of the plan, which has not been implemented yet, Pearson-Stuttard et al performed a microsimulation analysis using the US IMPACT Food Policy Model. That involved simulating the life course of a cohort of people ages 30 to 84 under the three different scenarios, with inputs taken from various published databases. Those scenarios were compared with no intervention, which assumed a continuation of the slow downward trend in sodium consumption from 3,150 mg/day in 2017 to 2,974 per day in 2036. Estimated sodium consumption in 2036 for the optimal, modest, and pessimistic scenarios were 2,224, 2,524, and 2,789 mg/day.
According to the simulation, there would be health and cost savings by 2036 for each of the three scenarios. In the optimal scenario, men and non-Hispanic black individuals would derive the most benefit.
Pearson-Stuttard pointed out that other countries have implemented similar policies and have seen population-level reductions in sodium intake and blood pressure. In the United Kingdom, for instance, a similar effort cut sodium intake by 8%, which was associated with a reduction in CVD events.
He said he hopes this study “will have a real impact in being able to inform the debate around the type of policy that the US might want to have toward sodium.”
He added that the study also “serves as another reminder to clinicians and to the public of just what a powerful risk factor sodium consumption is. And this should serve as a reminder to clinicians that you should continue to encourage your patients to reduce their sodium consumption, highlight the types of foods—so that’s processed foods predominantly—that your patients will be getting their sodium consumption from, and then that can make a real difference.”
Some Skepticism
Commenting for TCTMD, Andrew Mente, PhD (Population Health Research Institute, Hamilton, Canada), said he was unconvinced by the projections, calling into question the assumption that because reducing sodium intake lowers blood pressure, then it will also reduce cardiovascular events.
“The problem is that that assumption is not compatible with the data that we have on literally now hundreds of thousands of people across more than a dozen studies that looked at actual clinical events,” he said. “Not modeled outcomes but actual outcomes.”
He said that relying on a single risk marker—blood pressure—to determine the effect of reducing population-level sodium intake assumes that such an intervention would not have any other physiological effects. “But that is not a reasonable assumption at low levels of sodium,” he said, pointing to evidence that the renin-angiotensin-aldosterone system is activated in such a situation. Even at a level of intake around 2,200 mg/day—which the optimal scenario in this analysis achieved—there could be harm, Mente said.
A study published about 2 years ago by Mente’s group showed that the risk of a composite of death, MI, stroke, or heart failure was elevated in hypertensive and nonhypertensive individuals with a mean estimated sodium excretion below 3,000 mg/day as compared with 4,000 to 5,000 mg/day. Mente told TCTMD that intake between 3,000 and 5,000 mg/day should be considered the “sweet spot” at which risk of adverse outcomes is lowest.
Pushing back on Mente’s assertions, however, Pearson-Stuttard pointed to a 2014 meta-analysis by researchers led by Dariush Mozaffarian, MD, DrPH (Tufts University, Boston, MA), one of the authors of the current analysis, and said, “The literature is entirely consistent with reduced CVD mediated by [systolic blood pressure] reduction through reducing sodium. This is how we have modeled this, consistent with best evidence.”
He also highlighted a section of the current paper discussing the claim by Mente’s group that sodium consumption below 3,000 mg/day is harmful. The investigators say that “it appears that this argument is based on biased measurement methodology. In a recent discussion on the subject, Mozaffarian et al concluded that the optimal level of sodium consumption, below which further sodium reduction has no further health gains, is somewhere in the range of 614 mg/day to 2,391 mg/day.”
Thus, the claim that 3,000 to 5,000 mg/day is the “sweet spot” is “totally inconsistent with published literature,” Pearson-Stuttard said.
Of note, spokespeople from the American Heart Association (AHA), the American College of Cardiology, and the US Centers for Disease Control and Prevention all spoke up in support of the FDA’s 2016 draft guidance.
Waiting on the FDA
Pearson-Stuttard told TCTMD that after he presented some of these results at AHA’s EPI Lifestyle Scientific Sessions last month, the FDA reached out to learn more.
“They developed a really, really interesting and progressive policy, and here we’ve hopefully helped them by putting some numbers to the various different proposals they made,” he said.
The status of the agency’s guidance is uncertain, however. The 2018 Consolidated Appropriations Act signed into law last month prevents the agency from using funds for regulations or guidance aimed at food manufacturers for population-wide sodium reduction efforts “until the date on which a dietary reference intake report with respect to sodium is completed.”
Pearson-Stuttard said: “Our understanding is that it’s currently sort of paused. That these proposals were made, and there’s been no progress in implementing that proposal.”
When asked about the status of the plan, an FDA spokesperson pointed to a speech FDA Commissioner Scott Gottlieb, MD, gave at the National Food Policy Conference in Washington, DC, on March 29, 2018. In it, Gottlieb said “there remains no single more effective public health action related to nutrition than the reduction of sodium in diet.”
Gottlieb indicated that the agency’s focus, however, is now on the short-term voluntary sodium targets, which aim to reduce sodium intake to 3,000 mg/day. He said the agency is waiting to get information from the dietary reference intake report from the National Academies before moving forward with its own plan.
“Whether we fully align with that process, whether we incorporate it into some science-based assessment that we do on our own with respect to where that target should end up, I think that that’s going to be part of the process,” Gottlieb said during a question-and-answer session after his speech. “I think the important message is that we’re committed to continuing to move that process forward and we’re committed to continuing to take further steps to try to reduce that target amount.”
In a statement, AHA CEO Nancy Brown provided support for the population-wide approach put forth by the FDA.
“This change is something consumers say they want, and several major food companies have already been working to reduce sodium in many of their products. We commend those industry leaders and urge them to continue their efforts to give consumers more choice over the amount of sodium they eat,” she said. “It’s time for the FDA to level the playing field for food companies and advance the voluntary sodium targets. Adoption of these targets will save billions in healthcare costs and improve lives, which remains priceless.”
For his part, Mente urged caution “in the absence of any randomized controlled trial showing that low sodium at levels that they currently recommend is better than average sodium with regard to clinical events.”
While awaiting such a trial, he said, “before we divest large amounts of time and effort and resources to reducing sodium to levels that we have no idea what will result in as far as health in populations, it’s best we proceed with caution and instead focus on efforts to improving overall diet quality, like getting people to eat more fruits and vegetables for instance. That would be the optimal approach.”
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Pearson-Stuttard J, Kypridemos C, Collins B, et al. Estimating the health and economic effects of the proposed US Food and Drug Administration voluntary sodium reformulation: microsimulation cost-effectiveness analysis. PLoS Med. 2018;Epub ahead of print.
Disclosures
- The study was funded by grants from the National Institutes of Health.
- Pearson-Stuttard reports receiving personal fees from ICF strategic consulting unrelated to the study.
- Mente reports no relevant conflicts of interest.


Comments