First US Consensus Statement on PFO Closure Addresses Volume Requirements, Quality Measurements
The key to success will be ensuring a real-world patient population similar to those enrolled in the randomized trials, experts say.
The first US expert consensus document on patent foramen ovale (PFO) closure for cryptogenic stroke stresses the primary role that neurologists should play and suggests institutional and operator volume requirements.
This statement, published online last week in Catheterization and Cardiovascular Interventions, follows the publication of similar British and European recommendations published last year. All are rooted in the most recent data that have shown a clear benefit with the procedure in selected patients on optimal medical therapy compared with medication alone.
“It's kind of the end of the journey in trying to establish evidence for PFO closure, and I think it's very important that societies play a role in helping to shape the way practice is going to evolve in the United States,” writing committee chair Eric Horlick, MD (University Health Network, Toronto, Canada), told TCTMD.
Cardiologists and Neurologists
One of the primary goals with this specific document—which was sponsored by the Society for Cardiovascular Angiography & Interventions (SCAI) and affirmed by the American Academy of Neurology (AAN)—was to address and end the long-held contention between cardiologists and neurologists in this field, he said. “We really wanted to establish the neurologist as the gatekeeper [and] the importance of a partnership between neurology and cardiology,” Horlick explained.
That said, there aren’t enough trained vascular neurologists in the United States to meet the needs of every patient referred for PFO closure, he reported. “There's going to have to be compromise. [The] compromise is you have a community neurologist who's assessing someone for stroke and telling you what the etiology of the stroke is, and their level of expertise and comfort is not the same as a vascular neurologist who only sees stroke all day long.”
According to neurologist Steven Messé, MD (University of Pennsylvania, Philadelphia), who was not involved in crafting the new document, “the recommendation to have neurologists involved in the decision making for PFO closure was important and valuable.”
However, while he is “sympathetic to the concern that there are not vascular neurologists available in every center or locale where PFO closure may be considered,” Messé stressed in an email to TCTMD the importance of completing appropriate workups to determine the most likely stroke etiology for every patient, “regardless of whether PFO closure is being considered.” He added that he hopes that general neurologists will be “comfortable undertaking this challenge.”
In general, “performing the studies that were mandated for patients prior to enrollment in the PFO closure trials would be a reasonable approach,” Messé advised. “This includes brain MRI, head and neck vascular imaging (typically with CTA or MRA), and TTE/TEE. While it was not routinely performed during the period when PFO closure studies were ongoing, in appropriate patients I think that cardiac telemetry monitoring is important to rule out occult atrial fibrillation, and though not every study required it, it is worth considering hypercoagulable testing, though the yield of this testing, as well as how it impacts decision-making, is uncertain for most conditions.”
Specific Recommendations
The vast majority of the recommendations made in this document were created to reinforce performing PFO closure like it was in the randomized trials, Horlick said, noting that “we did leave some room to individualize care in specific situations.”
Primarily, the writing group emphasized that patient selection should mirror the enrollment criteria in the studies. “Patient selection should adhere closely to the FDA labeling which coincides with the inclusion criteria for the major RCTs,” they write. “The contemporary randomized trials of PFO closure only included patients with documented stroke 60 years of age or less and this is the subset of patients primarily included in the FDA labeling. Patients with transient ischemic attack (TIA) were not included.”
Additionally, Horlick and colleagues give specific guidelines for which operators and institutions should be performing PFO closure. To be initially qualified, operators should have a clinical knowledge base that includes “a comprehensive understanding” of stroke-related PFO closure and appropriate treatment strategies; “suitable training” on the FDA-approved PFO closure devices; an understanding of atrial anatomy and imaging; and experience with catheter-based management of potential complications. Operators should also have completed at least 50 structural/congenital catheter interventions with either a minimum of 25 septal interventions or 12 including PFO device placement.
In addition, they recommend new operators undergo a peer-to-peer training course and have a physician proctor for their first 10 interventions as well as for three to five cases involving new devices. Operators have to keep a 2-year volume of at least 30 procedures involving septal interventions or 15 cases of PFO device implantations to maintain their status as PFO closure proceduralists, the authors advise.
On top of the operator requirements, the authors suggest the following qualifications for institutions:
- More than 100 structural/congenital catheter interventions in the 2 years leading to PFO program initiation
- Yearly and thereafter, more than 50 structural/congenital interventions, at least 25 of which involved septal interventions and/or 12 specific to PFO device placement
- Continuous intraprocedural availability of a physician (interventional cardiologist, imaging cardiologist, or cardiac anesthesiologist certified in echocardiography and with experience in guiding structural/congenital heart interventions) with experience in TEE or intracardiac echocardiography in structural/congenital heart disease
- Multidisciplinary team that includes necessary staff and expertise for preoperative evaluation, performing the PFO closure procedure, and acute and long-term postprocedural follow-up
- Ready access to an active cardiothoracic surgery program with cardiac surgeons and perfusionists
- Cardiac catheterization laboratory, or hybrid room with hemodynamic monitoring and high-resolution imaging
The writing committee also proposed a set of quality assessment measures to monitor procedural safety and outcomes going forward. Notably, they say that if their operator and institutional requirements are met and that all patients are prescreened by both a cardiologist and neurologist, an acceptable procedure-related mortality rate would be below 1% and major bleeding would be below 5%. Also, postprocedural stroke would be below 1% and freedom from recurrent ischemic stroke at 1 year would be 100%.
“Another process measure of quality is the use of shared decision-making and the development of educational material for patients and families,” Horlick and colleagues write. “Best practices may include directing patients and family to an objective, noncommercial website for education. Decision aids could also be development to assist decision-making for patients facing the decision of whether or not to undergo PFO closure. These educational and decision-aids are not currently available but should be considered for future efforts by professional societies, individual sites, and other stakeholders.”
Looking Forward
While the FDA has mandated that manufacturers of approved PFO closure devices maintain registry data on patients going forward, Horlick questioned whether this kind of data collection would be ideal.
“It is the hope of the writing committee that a registry is formed to track immediate and long-term outcomes of patients undergoing PFO closure,” they write. “This registry should consider standardized follow-up, such as is done with the TVT registry. There are industry-sponsored ongoing FDA mandated postapproval studies that will follow patients out to 5 years. However, even 5-year follow-up may not be adequate for these young patients with many years of life ahead of them.”
“It's one thing for a company to collect data on their device. It's another thing to have an arm's-length group actually collect data,” Horlick stressed. “I'm saying it's something that needs to be considered, for sure. Anything that promotes quality is usually a good thing.”
“More data is usually a good thing,” Messé agreed. “I think that voluntary device/procedure registries rarely provide a very accurate view of what is going on, both in terms of who is getting the intervention and complication rates. That said, I think it would be interesting to see if people receiving PFO closure in clinical practice are similar to who was shown to benefit in the trials, and also if there appears to be a similar safety profile, acknowledging these limitations.”
Looking to the future, Horlick said that “now that there's an approved device and there's reimbursement, I think there's going to be a continued ramp up of the procedure to meet the needs of the US population.” While patients who were excluded from the trials, including the elderly, those with thrombotic disorders, and divers, will still need to be studied, “I think this was the most important hurdle,” he concluded.
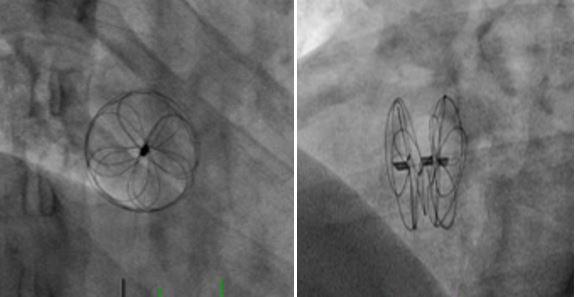
Photo Credit: Adapted from: Krishnaswamy A. PFO With Long/Well-Attached PFO Tunnel. Presented at TCT 2018, September 24, 2018. San Diego, CA.
Yael L. Maxwell is Senior Medical Journalist for TCTMD and Section Editor of TCTMD's Fellows Forum. She served as the inaugural…
Read Full BioSources
Horlick E, Kavinsky CJ, Amin Z, et al. SCAI expert consensus statement on operator and institutional requirements for PFO closure for secondary prevention of paradoxical embolic stroke. Catheter Cardiovasc Interv. 2019;Epub ahead of print.
Disclosures
- Horlick reports receiving institutional grant support from Abbott.
- Messé reports serving as a local PI for the REDUCE trial and as an investigator for the CLOSURE I trial.


Comments