European Guidelines Represent First Intersocietal Position on Percutaneous PFO Closure
Questions remain as to how to treat older patients and what exactly defines optimal medical therapy, but overall the paper is a helpful tool, experts say.
Highlighting an interdisciplinary approach and proper patient selection, a European task force has published what they claim to be the first intersocietal guideline consensus regarding percutaneous patent foramen ovale (PFO) closure in patients with cryptogenic stroke.
Their paper, published online last week ahead of print in the European Heart Journal, follows the publication of a similar British statement published in July; both come after years of research finally showing a clear benefit of the procedure in select patients alongside medical therapy compared with medication alone.
“Before this paper, there was no intersociety consensus about the treatment of PFO. This is the first official publication of international societies about that,” lead author Christian Pristipino, MD (San Filippo Neri Hospital, Rome, Italy), told TCTMD. “There were some guidelines, but they were really controversial. There were some neurological societies stating very narrow indications to percutaneous closure. Others were a little bit more open but they were [still] controversial. . . . For the first time it is clearly stated that percutaneous closure plus medical therapy is superior to medical therapy [alone] in high-risk patients.”
Interdisciplinary Approach, Diagnosis
The comprehensive document serves to guide decision-making in several circumstances, Pristipino explained. Primarily, he highlighted the importance the task force placed on an interdisciplinary approach to treating these patients.
Neurologist David Thaler, MD, PhD (Tufts Medical Center, Boston, MA), who was not involved with this paper, told TCTMD that this facet is vital to optimal patient care. “It's a problem when cardiologists get too far along on these issues without neurological input because the determination of the event itself, being stroke or something else, often requires some neurological sophistication, which is really I think in the purview of neurology rather than cardiology,” he said. Also, US Food and Drug Administration “labeling for these devices have suggested that both neurologists and cardiologists be involved in the diagnosis.”
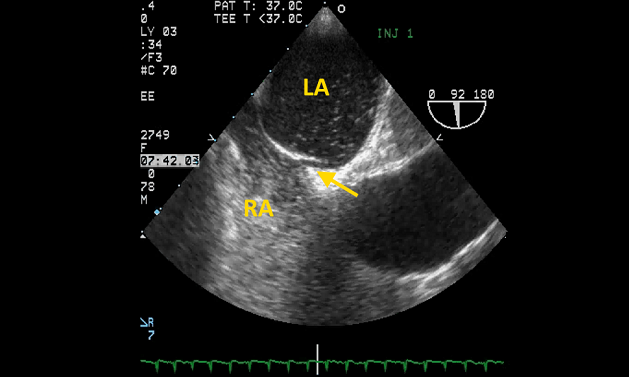
Additionally, Pristipino said the task force focused heavily on best practices for PFO diagnosis in the first place. Transesophageal echocardiography (TEE) has long been the “gold standard” for diagnosing PFO, he observed, “but unfortunately and deceivingly we found that in fact that the sensitivity of the technique is much less than what we thought before.” Therefore, the task force recommends contrast-enhanced transcranial Doppler as a first-line test to detect a right-to-left shunt, because of its high sensitivity. Transthoracic echo can be used as a first-line test, Pristipino clarified, noting that transcranial Doppler should be done afterwards if TTE is negative or equivocal. TEE should be used in all cases in which it is necessary to rule out embolic sources other than the PFO and to assess the anatomical features of a PFO, the authors state.
Thaler, who reviewed the algorithm set out in the paper for TCTMD, pointed out that “it's an open question about whether TEE is required before” a patient can be diagnosed with cryptogenic stroke. “You could argue that without a TEE, if you only have a TTE, you're going to miss a lot of potential embolic mechanisms,” he explained. “And so therefore if the TEE hasn't already been done then it's not cryptogenic, it's incompletely evaluated, which is a different stroke category.
“Having said that, I know that not everybody agrees with that position,” Thaler continued. “But I think you miss things without a TEE like aortic atherosclerosis with mobile thrombus, for example, or you miss a left atrial tumor or you miss thrombus in parts of the heart including the left atrial appendage and various other unusual mechanisms. So think it's an important test and that algorithm implies otherwise.”
Pristipino also noted that the task force aimed to emphasize the concept of “participative” medicine, with the patient involved in their treatment decisions as much as possible. For example, informed consent forms for percutaneous PFO closure should not be standardized. Rather “you need to build it together because every case is very particular and has specific characteristics. So you need to make an open form of consent,” and possibly also use narrative tools to enhance the patient’s understanding of their options, he said.
A Reasonable Guideline
Also commenting to TCTMD, Steven R. Messé, MD (Hospital of the University of Pennsylvania, Philadelphia), said the paper is “overall [a] reasonable guideline.” While he doesn’t agree with every single recommendation, he said, “I think that there is judgement in these things, and I understand where they're coming from. It is fairly comprehensive and, to some extent, I think it's giving permission to close peoples’ PFO who perhaps don't meet trial criteria. . . . So I think that there's a lot of wiggle room in the way they present the recommendations.”
Notably, the task force concluded the appropriateness of PFO closure in patients up to age 65, but the only study that has included patients over the age of 60 is DEFENSE-PFO. The evidence from that study is weak in comparison to the others, Messé said. “They didn't appear to adjudicate their outcomes, and so I don't really think there's as much evidence to support treating older patients yet. Obviously, I think that's something that we should be looking into more of, but to say as a blank guideline statement that we can consider closing anybody up to age 65 equally as you would a 20-year-old or 25-year-old, I don't think that necessarily would be correct. But again there's judgement involved in these things.”
Thaler also was concerned about another implication of the paper, namely, that the literature suggests that oral anticoagulation is better than antiplatelet drugs for stroke prevention even in patients who do not have their PFOs closed. He noted that several meta-analyses have been conducted without controlling for variables that lead to an anticoagulant or antiplatelet prescription. These studies “are probably fatally flawed, because the populations that end up getting anticoagulation are probably the same populations who have a lower baseline risk of recurrence anyway,” he explained.
While the task force recognizes that observational findings don’t carry the same weight as randomized trials, Thaler said that “nevertheless implying that we think oral anticoagulants are better than antiplatelet drugs is not actually consistent with the data that are available. . . . So I think that's still an open question which is of some importance, because if the implication is that anticoagulants are good enough and you don't need PFO closure, that means that the patient is going to end up on anticoagulation anyway.”
Open Questions
Overall, Thaler said these guidelines are likely to have an impact on practice. “I think it's going to help people to think through these patients. It's going to help cardiologists coordinate and collaborate with neurologists and other specialists like hematologists, and it may have an influence on national decision makers decisions about policy for PFO closure and whether they're going to cover them in their own national health care systems and so forth,” he predicted, adding that in the United States the document may also have an impact on insurance coverage.
“These kinds of papers can be helpful with changing attitudes,” Thaler continued. “A lot of insurers for devices like these or expensive medications or something won't cover things until guidelines are changed, not just because a study gets published. And so these kinds of things are more influential than perhaps they're meant to be, but I think they are important for that reason, too.”
Messé further pointed out that papers like these are useful for physicians struggling to make sense of the field. “I do think there are a lot of doctors out in clinical practice that don't have time to review all of these studies carefully, to assess the quality of the evidence, and to summarize all the data,” he said. “I think there's some question about whether it's helpful to have varying guidelines from multiple organizations that might not completely agree with one another and have some discordance. Some people find that challenging to understand, . . . but I also do think that it's important that you get different perspectives.”
It remains an open question about how to treat older patients with PFO who lack another explanation for an embolic recurring stroke, he said. NAVIGATE ESUS and RE-SPECT ESUS failed to show a benefit of rivaroxaban and dabigatran, respectively, over aspirin in the treatment of embolic stroke of undetermined source, Messé noted. The former “suggested that anticoagulation may benefit the patients who had PFO compared to aspirin,” and in the latter, “there wasn't a clear greater benefit in patients with a PFO, but the point estimate still favored it,” he commented. “So I do think there's this question about whether we should be anticoagulating older patients.”
Also, he said, “it would be reasonable to do a closure trial in older patients. The concern would be about increasing the A-fib incidence, as we know that's potentially a high-risk mechanism for stroke and the PFO closure devices do increase that risk as well even in younger patients where we've tried.”
Along with investigating which drug therapies are most useful, Pristipino said he would like to see more studies looking at which subgroups of patients “may benefit more from closure and [which] may benefit more so from medical therapy alone.”
The new data that have been published are “fairly compelling that there is a reduction in stroke risk. And by selecting your patients carefully, I think you're definitely going to be benefiting those patients to recommend closure,” Messé echoed. “The challenge there is to figure out which patients need to have their PFO closed.”
For now, Pristipino said he hopes this consensus document will help clarify decision-making regarding PFO cases worldwide and lead to a “more homogenous” approach.
Photo Credit: Steven R. Messé
Yael L. Maxwell is Senior Medical Journalist for TCTMD and Section Editor of TCTMD's Fellows Forum. She served as the inaugural…
Read Full BioSources
Pristipino C, Sievert H, D’Ascenzo F, et al. European position paper on the management of patients with patent foramen ovale: general approach and left circulation thromboembolism. Eur Heart J. 2018;Epub ahead of print.
Disclosures
- Pristipino reports no relevant conflicts of interest.
- Thaler reports serving on the steering committee of the RESPECT trial (AGA/St. Jude/Abbott) and the ongoing post-approval study (Abbott) and as a local investigator for the REDUCE trial.
- Messé reports serving as a local PI for the REDUCE and a subinvestigator for the CLOSURE I trial and conducting research with Gore not related to closure but aortic disease.


Comments