FLASH: More Data to Support Mechanical Thrombectomy in PE
RCTs are needed to see where the clot-retriever strategy “fits in” among other emerging treatment options, says Robert Bonow.
BOSTON, MA—A percutaneous mechanical thrombectomy device for pulmonary embolism (PE) improves hemodynamics and heart rate while patients are still in the procedure room, according to outcomes from the US cohort of the FLASH trial.
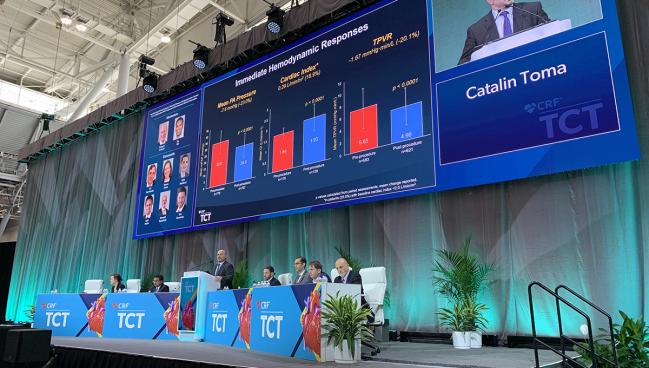
The clinical recovery seen soon after clot removal continued for 6 months, Catalin Toma, MD (University of Pittsburgh Medical Center Heart and Vascular Institute, PA), said in a press conference prior to his late-breaking presentation here at TCT 2022.
“Mortality remains high in the PE space, up to 10% at 30 days in recent registries, and hasn't changed that much,” Toma noted. “Perhaps much less appreciated is the comorbidity that these patients have, with high readmission rates and . . . quite a few patients having symptoms—up to 50%—in 3 to 6 months following acute PE.”
Unlike standard upfront lytic-based approaches that increase bleeding, he said mechanical thrombectomy can provide rapid resolution of the clot and relieve hemodynamic compromise without increasing the risk of serious bleeds. The data add to positive results from the FLARE study and the interim analysis of the first 500 patients in FLASH, suggesting that mechanical thrombectomy could be an option in a field that is heating up with newer catheter-based devices as well.
“We really need randomized trials to see where this fits in,” Robert O. Bonow, MD (Northwestern University Feinberg School of Medicine, Chicago, IL), said in the press conference. “This is a really important step forward with a different way of approaching the problem without giving antithrombotic therapies.”
Press conference moderator Roxana Mehran, MD (Icahn School of Medicine at Mount Sinai, New York, NY), pointed out that RCTs in this area, especially in acutely ill patients, are “a very difficult thing to do” in the United States. A key issue is consent, with Mehran adding that “going forward, we're going to have to have a way to get these patients consented even after the randomization, . . . and there is some move towards that so that we are able to actually perform these studies better.”
The results were simultaneously published in EuroIntervention.
US FLASH Cohort Results
The multicenter FLASH registry enrolled 800 PE patients in the US (and is enrolling 200 more in Europe) who were treated with the FlowTriever mechanical thrombectomy system (Inari Medical). The device consists of a catheter for aspiration of thromboemboli and a catheter for mechanical thrombus dislodgement and removal. After excluding one patient postenrollment who did not meet study criteria, the final US group consisted of 799 patients (mean age 61.2 years; 54% male; 25% Black) treated at 50 sites between December 2018 and December 2021. Of these, 92% had intermediate-risk (submassive) PE and 8% had high-risk (massive) PE. Concomitant deep-vein thrombosis (DVT) was present in 65% and approximately one-third had contraindications to thrombolytics.
The median thrombectomy time was 43 minutes. The majority of thrombectomy procedures were done via femoral access, with 86.6% of patients undergoing the procedure with anesthesia under sedation. No patients died during the procedure and access-site complications were rare, occurring in six patients. Prescribed anticoagulants after the procedure included new/direct oral anticoagulants (55.3%), vitamin K antagonist (5.3%), low molecular weight heparin (14.3%), and unfractionated heparin (30.0%).
At 48 hours, there were 14 major adverse events (1.8%), including 11 major bleeds. Two deaths were seen within 48 hours (one cardiopulmonary arrest and one new PE), which were not attributed to the device or procedure. Speaking with TCTMD, Toma said the latter situation, where a clot is in transit even as another is removed, is surprisingly common in this population of patients who tend to have concomitant DVT.
“We think it's most likely that that's how many of these patients die. They have one PE, they do relatively okay, and then they get a second embolization event or a third,” he said.
More than 60% of patients did not require an ICU stay following the procedure, which Toma told TCTMD he was happy to see. “The standard of care now when you have a massive or submassive PE is to send them to the ICU,” he said. “If they get lysed, they stay in the ICU for 2 or 3 days, so this is actually a good thing that so many of our patients did not need to be in the ICU after the procedure.”
Among the immediate hemodynamic improvements were a 7.6-mm Hg mean drop in pulmonary artery pressure from baseline (P < 0.0001) and a decrease in systolic pulmonary artery pressure of 23.4% (P < 0.0001). In further analyses, mean pulmonary artery pressure reductions were greatest in those with concomitant DVT and bilateral or saddle PE. Longer duration of symptoms, prethrombectomy systolic pulmonary artery pressure ≥ 70 mm Hg, and higher body mass index were associated with less robust decreases in mean pulmonary artery pressure.
Among patients with a depressed cardiac index, there was a 19% mean increase seen after the procedure. Total pulmonary vascular resistance decreased by a mean of 20%, and heart rate decreased by a mean of 11%. The mean right ventricle/left ventricle ratio also decreased from 66.5% to 15.6% (P < 0.0001). RV function improved in most cases, with 74.5% of patients having no or mild dysfunction by 48 hours. Patients also saw improvements in dyspnea and need for supplemental oxygen. At 30 days, the rate of all-cause mortality was 0.8% and the rate of PE-related readmission was 1.4%.
‘Ongoing Evolutionary Process’
To TCTMD, Toma said mechanical intervention could be lifesaving in patients with massive PE and contraindications to thrombolytics, and that it may be a good option for submassive PE patients who often are sicker than they appear and have the potential to do poorly when treated with heparin alone.
He said removing the clot effectively “resets the clock” for patients who often have suffered with shortness of breath for long periods of time. As for how RCTs of mechanical thrombectomy might shake out, he said in the submassive group, “the more important outcome is going to be improvement in their quality of life and how quickly they recover, since many of these patients are young.” The authors obtained only limited quality-of-life data from FLASH patients due to the COVID-19 pandemic.
Panelist Kenneth Rosenfield, MD (Massachusetts General Hospital, Boston), said the FLASH data set adds to the knowledge base on how to manage PE, which he called “an ongoing evolutionary process.” He specified that “the hardest thing for our PERT teams is deciding which way we should go,” in terms of choosing treatment strategies. But Rosenfield also said another challenge will be in choosing patients who are not candidates for something like mechanical thrombectomy.
While safety data are an important benchmark, panelist Eric A. Secemsky, MD (Beth Israel Deaconess Medical Center, Boston, MA), noted that given that the devices can be difficult to deliver and bleeding complications can occur, real-world operators will be looking at this new technology in terms of the learning curve and from the perspective of practical issues when using it in their lab.
“Very often we have trouble approaching [mechanical thrombectomy] from the femoral and we switch to a different access site, and utilize other tools . . . to try to augment the success of the procedure,” he added.
Toma said the learning curve based on operator requirement to be part of FLASH was five procedures, but emphasized that even though he does many of these procedures himself, he too is still learning. This is not surprising, Toma noted, given how new this field and these devices are for interventional operators.
L.A. McKeown is a Senior Medical Journalist for TCTMD, the Section Editor of CV Team Forum, and Senior Medical…
Read Full BioSources
Toma C, Jaber WA, Weinberg MD, et al. Acute outcomes for the full US cohort of the FLASH mechanical thrombectomy registry in pulmonary embolism. EuroIntervention. 2022;Epub ahead of print.
Disclosures
- Toma reports consulting for Medtronic and Philips.





Comments