FORZA: For Intermediate Lesions, OCT-Guided PCI Costs More, Yields Better Outcomes vs FFR
“These techniques are complementary and each offer different, important information,” William Fearon says.
SAN FRANCISCO, CA—For patients with angiographically-intermediate coronary lesions, optical coherence tomography (OCT) and fractional flow reserve (FFR) each can guide PCI. But as confirmed by the FORZA randomized trial, the two tests offer different benefits, with OCT holding a slight edge.
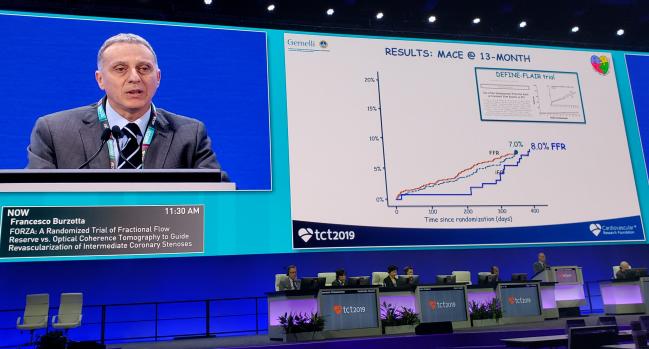
At 13-month follow-up, OCT was linked to a lower combined rate of MACE and significant angina, the single-center study’s primary endpoint, whereas FFR was associated with a higher rate of medical management and lower costs. In the OCT group, the decision for or against PCI was based on minimal lumen area and percent diameter stenosis.
“The decision whether to treat or conservatively manage patients with angiographically-intermediate coronary lesions represents a major clinical issue,” said co-principal investigator Francesco Burzotta, MD, PhD (Università Cattolica del Sacro Cuore, Rome, Italy), during a late-breaking science session at TCT 2019. The results were simultaneously published online ahead of print in JACC: Cardiovascular Interventions. Last year, the FORZA investigators reported 1-month data at TCT.
As the researchers note in their paper: “Major international clinical guidelines on myocardial revascularization support the use of physiological assessment to guide revascularization in patients with angiographically-intermediate coronary lesions. Yet, intracoronary imaging techniques are raising growing interest.” FFR is done upfront to decide whether and where PCI is needed, whereas OCT is done post-PCI to check whether stents are optimally expanded.
FORZA was designed as a head-to-head comparison to add clarity on the best strategy, Burzotta said, with the hypothesis that OCT would be superior.
William Fearon, MD (Stanford University School of Medicine, CA), a panelist in the session, told TCTMD that FORZA “reinforces the importance of doing FFR upfront to avoid unnecessary stents and to do a cost-effective approach [then using] OCT to optimize your deployment.” Yet it also “highlights some of the limitations of both technologies,” Fearon observed, adding, “These techniques are complementary and each offer different, important information.”
The morphology of the plaque and the minimal lumen area in combination are in fact very, very relevant. Ziad Ali
Commenting on the findings for TCTMD, Ziad Ali, MD (NewYork-Presbyterian/Columbia University Irving Medical Center, New York, NY), described FORZA as “really exciting.”
“There are not a lot of completely uncharted territories that are currently under question in interventional cardiology,” he said. Pitting physiology against imaging in this way has not been done before, Ali stressed. Although the study is small and has certain limitations, among them setting the bar for statistical significance as a 50% decrease in the primary endpoint, “it is a randomized controlled trial in intermediate lesions and imaging came up ahead” overall, Ali asserted.
To him, this makes the case that “the coronary artery is not just a tube, it’s a biological tube. The morphology of the plaque and the minimal lumen area in combination are in fact very, very relevant. That makes sense,” he noted, adding that while the cost of OCT is higher, its use “does appear to have a clinical benefit at 13 months.”
FORZA sets the stage for further research comparing physiological assessment and intravascular imaging, Ali said.
Anatomy Versus Physiology
Burzotta et al enrolled 350 patients with 446 angiographically-intermediate lesions, randomizing them to OCT or FFR. With OCT, PCI was done if the area stenosis was at least 75% or was 50% to 75% with a minimal lumen area < 2.5 mm2. With FFR, PCI was performed for lesions with values ≤ 0.80. Baseline characteristics were similar apart from more previous MI in the OCT group and more left anterior descending artery involvement in the FFR group.
By 13 months, the primary composite endpoint of MACE (death, MI, or TVR) or significant angina (Seattle Angina Questionnaire frequency scale < 90) was lower in the OCT arm than in the FFR arm: 8.0% vs 14.8% (P = 0.048). The result was driven by nonsignificant trends in individual components that together added up to a significant difference. Notably, however, the secondary endpoint of target vessel failure (any MACE not clearly related with another vessel) was reduced with OCT compared with FFR (2.3% vs 7.4%; P = 0.027).
“In patients with angiographically-intermediate coronary lesions suitable for invasive evaluation by either OCT or FFR, the choice of one technique instead of the other may significantly affect the clinical course,” the researcher note. With FFR compared with OCT guidance patients were more apt to initially receive medical management (67.7% vs 41.1%), and this continued to be the case through 13 months (62.5% vs 44.8%; P < 0.001).
Total costs were also lower with FFR (mean 2,577 vs 3,750 Euros; P < 0.001). As previously reported, the FFR arm involved lower use of balloons/stents, lower contrast volume, and fewer cases of acute kidney injury.
Fearon pointed out that the events weren’t independently adjudicated and that the study wasn’t blinded. “Some of the harder endpoints did trend in the right direction for OCT, but not significantly. So I think it’s hard to draw firm conclusions about [outcomes]. The primary endpoint just barely met statistical significance and included a weak endpoint with angina, so it’s hard to know for sure what all that means,” he said.
In discussion following Burzotta’s presentation, Fearon asked: “My question is, are you proposing that we should choose one [test] over the other? In my mind it would seem that both work together and provide different information that overall optimizes PCI.”
Burzotta replied by noting that Fearon had put the results in the “correct perspective.” Large randomized trials have established that FFR is a very useful tool, but OCT can provide additional details, especially in instances of negative FFR values, he said.
The way of the future, Ali suggested to TCTMD, may be a technology such as CT-derived FFR that blends intravascular imaging and physiological assessment, one that could visualize plaque characteristics, measure ischemia, and assess whether stenting has resolved it.
Caitlin E. Cox is Executive Editor of TCTMD and Associate Director, Editorial Content at the Cardiovascular Research Foundation. She produces the…
Read Full BioSources
Burzotta F, Leone AM, Aurigemma C. Fractional flow reserve or optical coherence tomography to guide management of angiographically-intermediate coronary stenosis: a single-center trial. J Am Coll Cardiol Intv. 2019;Epub ahead of print.
Disclosures
- Burzotta reports receiving speaking fees from Abbott, Medtronic, and Abiomed.
- Fearon reports receiving research support from Abbott and Medtronic, having minor stock options with HeartFlow, and being a consultant for CathWorks.
- Ali reports receiving grants from Abbott and CSI; receiving honoraria from Boston Scientific, AstraZeneca, Opsens, Cardinal Health, and Acist; and having equity in Shockwave.


Comments