High Rate of Residual Ischemia After PCI Despite Excellent Angiographic Outcomes: DEFINE-PCI
The use of iFR could identify other focal lesions, thereby reducing residual ischemia and potentially cutting recurrent events after PCI, say experts.
NEW ORLEANS, LA—Despite successful PCI and optimal angiographic outcomes, nearly one in four patients leave the catheterization lab with some degree of residual ischemia, according to the results of a new study.
With a better assessment of coronary physiology post-PCI, however, physicians could reduce the number of significant lesions left behind after stenting and potentially trim the risk of recurrent ischemic events, say researchers.
“Even though we think we do a good job based on the angiogram, the angiogram isn’t totally reliable,” lead investigator Allen Jeremias, MD (St. Francis Hospital, Roslyn, NJ), told TCTMD. “We leave behind a fair amount of residual ischemia despite us thinking we did a good job. If we had this information available, and it was used routinely, in the vast majority of cases we could improve the acute outcomes or at the very least improve the physiology, which we think will translate into better outcomes long-term.”
Presenting the main results of DEFINE-PCI on March 17, 2019, at the American College of Cardiology 2019 Scientific Session, Jeremias said that recurrent angina after PCI is quite prevalent in most PCI trials, ranging from 20% to 30% at 1 year. “It’s not a small population,” he said. “At the same time, we also know from studies where [fractional flow reserve (FFR)] has been done—physiology assessed after PCI—there is a substantial number of cases, maybe around 20% or so, with significantly impaired physiology even when we think we did a good job on the angiogram.”
Sukhjinder Nijjer, MD, PhD (Imperial College, London, England), one of the study investigators, said DEFINE-PCI is unique as it shows how the instantaneous free-wave ratio (IFR) and iFR “pullback,” which is a pressure map of the entire coronary vessel, could be clinically meaningful.
“These data are exciting because it may explain why our PCI studies have not shown dramatic improvements in angina or outcomes: perhaps because more work was needed within the vessel,” Nijjer said via email. “It’s striking that the 24% residual ischemia is similar to the numbers of recurrent angina in a large number of PCI studies, including COURAGE, FAME, FAME 2, and SYNTAX.”
iFR Pullback and Residual Ischemia
The purpose of DEFINE-PCI was to determine how often patients leave the cardiac catheterization laboratory with significant residual ischemia despite operators achieving excellent angiographic outcomes. In total, 500 stable and unstable angina patients with a baseline iFR value of less than 0.89, indicative of physiological impairment, underwent PCI.
Following PCI, investigators repeated the iFR and iFR pullback in a blinded fashion (it was not used to optimize the procedure). Whereas iFR is a spot assessment of ischemia, the iFR pullback is created when the wire is slowly pulled back to create a physiological map of lesion severity. To TCTMD, Jeremias explained that iFR pullback can identify “step-ups,” which occur when the transstenotic pressure gradient is higher in different locations as the wire is pulled back across the vessel. The increased pressure gradient might be explained by a missed focal lesion or diffuse atherosclerotic disease, he said.
Mean iFR increased from 0.69 at baseline to 0.93 after the completion of PCI (average change 0.24). Of the 467 patients who had successful PCI—defined as operator-assessed residual diameter stenosis less than 50% in any treated lesion—24% had an iFR ≤ 0.89, which is hemodynamically significant. The good news, however, is that the vast majority (81.6%) of physiologically significant lesions left behind were focal stenoses rather than diffuse disease, said Jeremias. Of the 93 vessels with residual focal disease, the “physiologic miss” was observed equally in segments distal and proximal to the implanted stent.
“This means that they could be potentially fixed,” said Jeremias. “We estimated that if all residual focal lesions could be treated with additional PCI, which is obviously somewhat speculative, the rate of significant ischemia would be reduced from 24% to 5%.”
To TCTMD, Nijjer pointed out that while many cardiologists use iFR or FFR to confirm an ischemic vessel, they rely on the angiogram when selecting the stenosis for stenting, which can be misleading. In the past, when operators identified significant post-PCI residual ischemia with FFR or iFR, it is often attributed to diffuse atherosclerotic disease. DEFINE-PCI shows that’s not the case, and that the identified ischemia could be resolved with further intervention, said Nijjer.
No Correlation Between Angiogram and Post-PCI Physiology
The investigators observed no significant correlation between angiographic diameter stenosis and post-PCI physiologic measures. Nearly 30% of patients with a residual diameter stenosis ≥ 50% on angiography had an iFR ≤ 0.89. For those with a residual diameter stenosis less than 50%, more than 21% had an iFR ≤ 0.89 (P = 0.24).
In terms of the big picture, Jeremias believes iFR and iFR pullback could be helpful to address physiologically significantly lesions in need of PCI. The DEFINE-Guided Physiologic Stenting (GPS) study, sponsored by Royal Philips, will soon be launched and that trial will randomize patients to an IFR-guided therapy with pullback or to angiographically-guided PCI (with optional intravascular ultrasound).
For Nijjer, the DEFINE-GPS study will allow operators to have access to the iFR-pullback data to help achieve the best physiological result. “When we systematically and routinely use iFR-pullback, particularly when co-registered with the angiogram, we often see that the lesion we think is the most important in fact doesn’t contribute to the greatest pressure loss in the vessel,” he said. “Having this data upfront should allow interventional cardiologists to know what lurks within the vessel, before performing their PCI.”
John Warner, MD (UT Southwestern Medical Center, Dallas), one of the discussants during the featured clinical research session, said the evidence of residual ischemia after PCI challenges, once again, the definition of angiographic success. He pointed out that it remains a challenge to assess atherosclerosis at the end of stented segments.
“When you look at where the angiographic miss is, and the fact it correlates with physiologic miss in terms of residual ischemia, it’s a fascinating finding that deserves further exploration,” said Warner. “I think for patients with diffuse disease, additional evaluation with iFR could be very helpful in the decision-making pathway, both preangioplasty and certainly once you’re finished.”
In the trial, physicians used IVUS in roughly 10% of cases, and Jeffrey Moses, MD (NewYork-Presbyterian/Columbia University Irving Medical Center, New York, NY), questioned whether its ancillary use had any effect optimizing PCI and limiting residual stenosis. Jeremias said that they plan to publish those findings but have not yet completed the analysis.
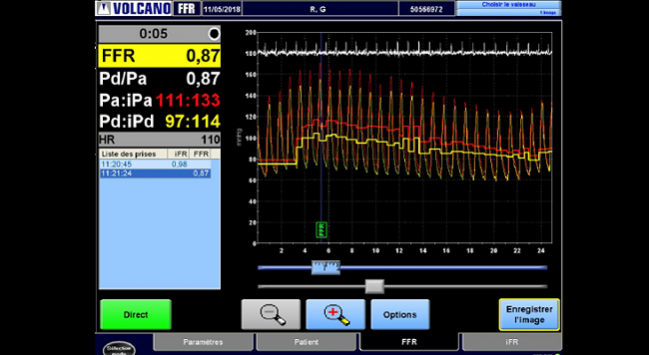
Photo Credit: Adapted from Monsegu J. Pro iFR! Presented at: TCT 2018. September 24, 2018. San Diego, CA.
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Jeremias A, on behalf of the DEFINE PCI investigators. Blinded physiological assessment of residual ischemia after successful angiographic PCI. Presented at: ACC 2019. March 17, 2019. New Orleans, LA.
Disclosures
- Jeremias reports institutional grants from Volcano/Philips and Abbott Vascular and consulting fees/honoraria from Volcano/Philips, Abbott Vascular, Opsens, Boston Scientific, Chiesi, and AstraZeneca.


Raymond Ellis