Human Papilloma Virus May Contribute to CVD Risk in Women, Korean Study Finds
Among healthy, middle-aged women, the interaction between HPV and CV events was strongest in those who were obese or had metabolic syndrome.
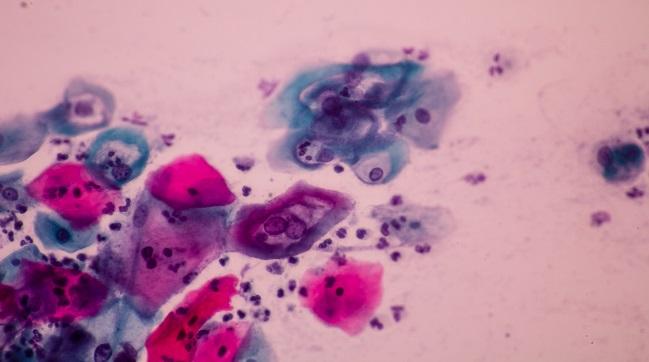
Some strains of human papilloma virus (HPV) may increase the risk of ischemic heart disease and stroke in women, new research suggests.
“Our study findings indicate the high-risk HPV infection may contribute to the development of CVD when accompanied by obesity or metabolic syndrome,” said the study’s senior author, Seungho Ryu, MD, PhD (Sungkyunkwan University School of Medicine, Seoul, Korea), in an email.
An association between the presence of HPV, the most common sexually transmitted infection in the world, and CVD was first reported in 2011 in a study of women in the National Health and Nutrition Examination Survey (NHANES). While that study suggested a causal link based on self-reported data, it did not provide evidence that having HPV led to a higher risk of being diagnosed with CVD.
In a study published online February 7, 2019, in Circulation Research, Ryo and colleagues add to the hypothesis by showing that even after adjustment for known cardiovascular risk factors, women with high-risk strains of HPV that have been linked to cervical, anal, and oropharyngeal cancers remained at higher risk of incident CVD than those without HPV infection (adjusted HR 1.22; 95% CI 1.01-1.49). The association even remained after adjustment for high-sensitivity C-reactive protein.
To TCTMD, Ryo said better understanding of high-risk HPV as a risk factor for cardiovascular events, as well as more insight into the possible synergistic effect of having high-risk HPV, obesity, and metabolic syndrome, may help improve preventive strategies and patient outcomes.
Too Soon for Routine Testing
The study involved 63,411 women aged 30 and older who underwent comprehensive wellness exams yearly or every other year between 2011 and 2016 that included testing for high-risk HPV. The overall incidence of HPV in the cohort was 7.6%, which the researchers note is low in comparison to the United States, where the prevalence in women of the same age is estimated at 14% to 19%.
Compared with nonobese HPV-negative women, those who had a body mass index of 25 kg/m2 or greater and had high-risk HPV infection had an increased risk of new-onset CVD events (adjusted HR 1.73; 95% CI 1.19-2.51), with a strong statistical correlation for obesity (P for interaction = 0.002). Similarly, women with high-risk HPV and metabolic syndrome had higher rates of new-onset CVD events than those without metabolic syndrome or HPV (adjusted HR 1.99; 95% CI 1.28-3.08); however, the correlation did not reach statistical significance (P for interaction = 0.05).
According to Ryu and colleagues, the exact mechanisms by which high-risk strains of HPV may contribute to CVD is not fully understood, but some HPV proteins have been isolated from the coronary arteries in cadaver studies and have been implicated in the development of atherosclerosis.
For now, Ryu told TCTMD, it is too premature to recommend HPV testing as a routine part of CVD risk assessment “since further studies are required to confirm the causal relationship of high-risk HPV infection with CVD risk.” Also unknown is whether there is a similar correlation between HPV infection and CVD in men.
L.A. McKeown is a Senior Medical Journalist for TCTMD, the Section Editor of CV Team Forum, and Senior Medical…
Read Full BioSources
Joo E-J, Chang Y, Kwon M-J, et al. High-risk human papillomavirus infection and the risk of cardiovascular disease in Korean women: a cohort study. Circ Res. 2019;Epub ahead of print.
Disclosures
- The study authors report no relevant conflicts of interest.


Comments