Hybrid Surgical/Interventional LV Reconstruction Improves Ejection Fraction and Patient Symptoms
Although it’s early and the data are slim, using anchors to plicate and excide the fibrotic tissue appears to offer some promise for ischemic HF.
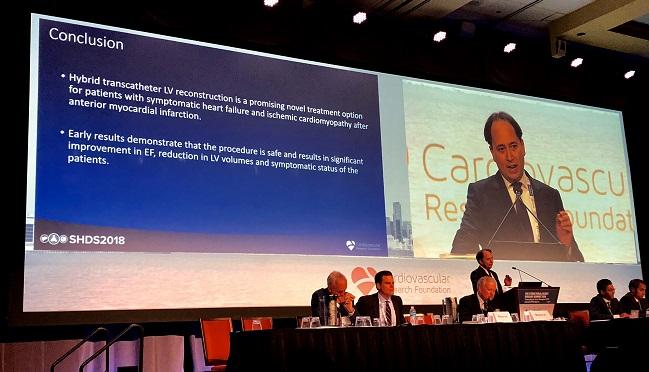
CHICAGO, IL—An unconventional approach to combat left ventricular remodeling following myocardial infarction appears to improve heart function and patient symptoms, although investigators caution it’s still early days for the new ventricular reconstruction procedure.
The hybrid transcatheter technique, which involves an interventional cardiologist and cardiac surgeon reconstructing the remodeled left ventricle by essentially folding over the fibrotic scar to take it out of play, led to an increase in the left ventricular ejection fraction and stroke volume, as well as improved NYHA symptom status in extended follow-up.
“I think the concept is pretty good and we’re really happy with the results,” lead investigator Patrick Klein, MD (St. Antonius Hospital, Nieuwegein, the Netherlands), told TCTMD.
Presenting early clinical experiences with the technology at the 2018 Structural Heart Disease Summit, Klein started by offering a primer on left ventricular remodeling after a large myocardial infarction. Large infarcts can lead to changes in left ventricular shape and function, he noted, such that the normally elliptical left ventricle becomes spherical and dilated. The transmurality of the myocardial scar—a transmural MI involves the full thickness of the myocardium—determines whether a left ventricular aneurysm develops, he added. In such cases, the portion of muscle with the aneurysm no longer contracts, which decreases heart function and leads to congestive heart failure.
“Normally you treat these patients with optimal medical therapy, and if any valvular problems arise, then you treat the valve,” Klein told TCTMD. “But we don’t really do anything for the ventricle to make the volume smaller. By making the volume smaller, we can decrease wall stress and increase the ejection fraction. It’s like a direct remodeling technique, which is very interesting for patients with ischemic heart failure after myocardial infarction.”
Surgical reconstruction of the left ventricle is an invasive procedure, added Klein, and the results are mixed. For example, in the STICH trial, adding surgical ventricular reconstruction to CABG surgery did not reduce mortality or hospitalizations for heart failure compared with bypass surgery alone in patients with ischemic heart failure.
To TCTMD, Klein said the reduction of the left ventricle in the STICH trial was likely too small to achieve a significant treatment effect. “If you only take out a small part of the apex, and don’t do much to decrease the volume of the ventricle, it’s not really remodeled,” he said.
Scars and Anchors
With their hybrid transcatheter approach, which doesn’t require sternotomy or cardiopulmonary bypass, a 14-Fr introducing sheath is first inserted into the right jugular vein and the snare is eventually deployed into the right ventricular outflow tract.
For the second step, an 18-gauge straight needle is inserted into the lateral scar, through the septum, to deliver a guidewire to the snare. This creates a protected wire rail through the heart to deliver the anchors. The anchors—an interior anchor attached to the scar on the right ventricular side of the septum and the external, mating anchor attached from the epicardial surface—are then used to plicate the scar and reduce the left ventricle volume.
In essence, the team reconstructs the left ventricle by pulling the anterolateral scar into contact with the septal scar, the intention being to exclude the large dyskinetic intervening segment from viable tissue.
“When you first see it, you think there’s a lot of steps, but for a lot of our colleagues in interventional cardiology, I think snaring is pretty straightforward,” said Klein. “The crucial part is the reconstruction. For the surgeon who wants to do the plication of the heart needs to think about how to place the anchors. Because the surgeon does half, and the cardiologist does half, I don’t think it’s that difficult.”
The early results look promising, he said. Among the 12 patients treated at their center, the researchers saw a postoperative improvement in left ventricular ejection fraction and left ventricular volumes. There was also an improvement in symptoms over time, with all 12 patients reported to have NYHA class 1-2 symptoms an average of 287 days after the procedure. Comparatively, 10 of the 12 patients had NYHA class 3-4 symptoms prior to ventricular reconstruction.
The panel, including session moderator Martin Leon, MD (NewYork-Presbyterian/Columbia University Irving Medical Center, New York, NY), called the procedure “very, very provocative,” and turned to the surgeons for their take on the early clinical data. For his part, surgeon Isaac George, MD (NewYork-Presbyterian/Columbia University Irving Medical Center), initially joked that he was on vacation when the complicated procedure was taught, but said there is precedent, such as with the Coapsys device to treat functional mitral regurgitation, to support therapies that affect left ventricle size and dimensions.
“Doing something externally has worked,” said George. “The constraint devices all have good data so if we can get [hybrid approach] to work, I think there’s potential. It’s something to be explored.”
Hemal Gada, MD (UPMC Pinnacle, Harrisburg, PA), who was not involved in the study, told TCTMD the treatment approach does address an unmet need in clinical practice and that he looks forward to future device iterations that can simplify the procedure.
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Klein P, Agostoni P, Swaans, MJ. Early clinical experience with hybrid transcatheter left ventricular reconstruction for the treatment of ischemic heart failure. Presented at: Structural Heart Disease Summit. June 22, 2018. Chicago, IL.
Disclosures
- Klein reports consulting fees/honoraria from BioVentrix and Edwards Lifesciences.


Comments