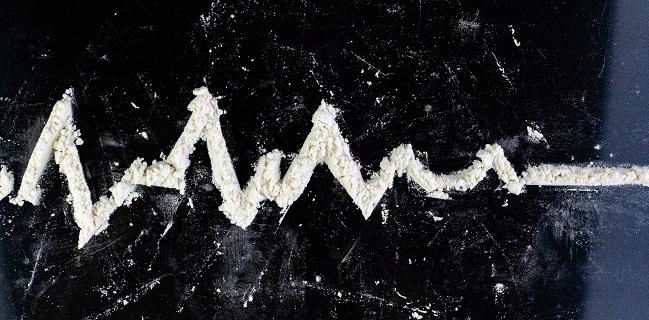
Invasive Approach Best for Cocaine-Linked NSTEMI, but DAPT Is Key
Because of the risk of stent thrombosis, the threshold to stent needs to be very high if a patient is likely to be nonadherent.
Patients with a history of cocaine use who present with non-ST-segment elevation myocardial infarction have a lower risk of future major adverse cardiovascular events if treated invasively rather than with a more-conservative approach, according to a new retrospective study.
Overall, invasive management, which included coronary angiography followed by PCI or CABG if needed, lowered the risk of MACE at 6 months by 28% compared with a noninvasive strategy.
The results, however, point to one of the major challenges in treating patients with cocaine-associated NSTEMI, namely their ability to adhere to posttreatment dual antiplatelet therapy (DAPT). While there was no greater risk of emergent revascularization in the overall cohort, that risk was significantly elevated among patients deemed nonadherent to medical therapy who’d been treated with a drug-eluting stent, report researchers.
“My threshold to take these patients to the cath lab has significantly decreased, meaning that it’s not unreasonable to cath these patients because you will find significant coronary artery disease,” senior investigator Mehdi Shishehbor, DO, PhD (Harrington Heart and Vascular Institute/Case Western Reserve University School of Medicine, Cleveland, OH), told TCTMD. “Many of them have significant comorbidities. Now, once you cath them, with the decision to revascularize them, you need to be very mindful, very careful, and very thoughtful. You need to take into consideration whether the patient is going to be compliant [with medical therapy] or not.”
That’s a conversation that can’t happen when the patient is on the cath lab table, he added.
“You need to talk them, to get to know their family before you take them to the cath lab,” said Shishehbor. “These are NSTEMIs, so there is no urgency, but I think it’s extremely important as interventionalists and as physicians that we learn more about these patients, understand their environment, and make sure we get them social support, and get them to the right people who can work with them so they can take their medication.”
If a patient with a history of cocaine use presents with STEMI, revascularization is an easy call, he added. However, with NSTEMI, depending on the patient’s symptoms and extent of troponin elevation, it can be misinterpreted as vasospasm or a type 2 MI caused by hypertension.
The current paper, published March 15, 2021, in JACC: Cardiovascular Interventions, came about after Shishehbor rounded with fellows, including lead author Shilpkumar Arora, MD (Case Western Reserve University School of Medicine), and ended up debating how to best care for a patient with NSTEMI who had used cocaine that morning.
Invasive Treatment Best, but Medication Critical
In 2008, the American Heart Association (AHA) published recommendations for the management of cocaine-associated chest pain and MI, noting the illicit drug has multiple cardiovascular and hematologic effects that can contribute to myocardial ischemia and/or MI. For example, cocaine increases heart rate and blood pressure, and even at small doses it is associated with vasoconstriction of the coronary arteries. The drug stimulates platelet activation and causes endothelial dysfunction, all of which can lead to accelerated obstructive atherosclerosis.
Still, the ideal treatment of cocaine-associated NSTEMI isn’t clear: there are no randomized, placebo-controlled trials in this setting. In 2014, the American College of Cardiology (ACC) and AHA recommended that patients with NSTE ACS and a recent history of cocaine use be treated the same as those with NSTE ACS who don’t use illicit drugs. However, that recommendation is based only on expert opinion and case studies (class I, level of evidence C).
In this retrospective series, the researchers obtained data from the Nationwide Readmissions Database in 2016 and 2017. The study included 3,735 patients (mean age 53 years; 78.2% women) with NSTEMI and a history of cocaine use. More than 80% of patients were tobacco users, 80% had hypertension, and 70% had prior history of coronary artery disease. After propensity matching, they identified 2,174 pairs treated invasively or with medical therapy.
After a median follow-up of 6 months, the risk of MACE was significantly lower among patients who underwent coronary angiography (HR 0.72; 95% CI 0.56-0.92). The benefit was driven by a significant reduction in the number of readmissions for MI (HR 0.64; 95% CI 0.48-0.85). In terms of the safety, there was no significant difference in the risk of emergent revascularization between the two approaches.
Next, the researchers assessed outcomes among patients treated with coronary revascularization compared with those treated noninvasively. Here, among 746 matched pairs, the risk of MACE was significantly lower for those who underwent PCI or CABG (HR 0.54; 95% CI 0.40-0.73) compared with a noninvasive approach, and this benefit associated with reduced readmissions for MI. When analyzing outcomes by revascularization strategy, PCI and CABG surgery were both associated with significant reductions in the risk of MACE, whereas the risk of emergent revascularization was significantly elevated with PCI (HR 1.78; 95% CI 1.12-2.81)—not with CABG—compared with the noninvasive strategy.
Given the heightened risk of emergent revascularization in the PCI-treated patients, the researchers performed a subgroup analysis based on adherence to guideline-directed medical therapy. While the cumulative MACE rate was not significantly different between the medically nonadherent PCI- and CABG-treated patients, the need for emergent revascularization was 4.5 times higher among those treated with PCI (HR 4.45; 95% CI 2.07-9.57). For nonadherent surgical patients, though, there were no safety concerns.
To TCTMD, L. Kristin Newby, MD (Duke Clinical Research Institute, Durham, NC), who co-authored the AHA scientific statement on the management of cocaine-associated chest pain and MI, said these patients tend to present quite young compared with conventional MI cases. With cocaine use, cardiac biomarkers might be elevated for reasons not related to plaque rupture, but chronic use of cocaine can precipitate early-onset coronary artery disease, she noted. For patients with chest pain and a history of cocaine use, it’s important to have a high index of suspicion for MI, particularly if they have multiple risk factors for coronary artery disease, said Newby.
“It makes sense that we would treat them like any other non-STEMI, including an early invasive strategy,” said Newby, adding that randomized trials showing an early versus delayed strategy for NSTEMI show an advantage for early treatment, particularly for reducing reinfarctions. “It makes sense that would apply in patients with cocaine use, particularly if you’re being somewhat selective,” such as applying the invasive strategy to NSTEMI patients with other risk factors or high-risk ECG changes, she noted.
If a person with admitted cocaine use has been into the hospital multiple times for chest pain and has already been sent to the cath lab once, it’s very unlikely the next time is going to be a coronary blockage, added Newby. “The first time makes sense to document the anatomy, and if the anatomy looks normal, then you feel pretty good about the next time they come in.”
High Threshold for DES
Shishehbor said that if physicians are reasonably sure the patient will comply with medical therapy, PCI is an option depending on the anatomy, as is CABG surgery. With surgery, though, the need to adhere to medical therapy afterwards is less critical given the risks of stent thrombosis following PCI.
If the patient is likely to be nonadherent, “then the threshold to put a stent in should be high,” he said, adding that you might not be doing the patient any favors with a DES if they won’t, or can’t, comply with DAPT. “It’s easy to take a patient to the lab, do a left-heart catheterization, and put in a stent, but if they don’t take their medication, don’t take their dual antiplatelet therapy, now you’re dealing with stent thrombosis, which could be much worse,” said Shishehbor.
Newby agreed. “If you’re putting stents into people’s arteries, adherence to therapy becomes super important,” she said. “There’s always that factor in many of these patients, that they’re not as adherent to therapy as we would hope.”
In an editorial, Debabrata Mukherjee, MD, and Richard Lange, MD (Texas Tech University Health Sciences Center, El Paso), say that finding—nonadherence to medical therapy is associated with higher risks of emergent revascularization in those treated with PCI—is a “clinically significant finding.” For their part, the editorialists agree with the ACC/AHA recommendations that cocaine-associated MI should be managed similarly to the broader population. “We think clinicians should also factor in possible medication adherence issues when deciding on revascularization in these individuals,” they advise.
Getting the patient to quit using cocaine should be the primary goal of secondary prevention in this setting, among other aims, according to Mukherjee and Lange.
“Patients who have been treated for cocaine-associated MI should advance to secondary prevention of atherosclerotic cardiovascular disease with antiplatelet drugs and high-intensity statin therapy, and may require additional medications depending upon the extent of myocardial damage from the MI such as angiotensin-converting enzyme inhibitor or angiotensin receptor blocker for heart failure,” they write.
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Arora S, Jaswaney R, Jani C, et al. Invasive approaches in the management of cocaine-associated non-ST-segment elevation myocardial infarction. J Am Coll Cardiol Intv. 2021;14:623-636.
Mukherjee D, Lange RA. Management of cocaine-associated non-ST-segment elevation myocardial infarction: is an invasive approach beneficial? J Am Coll Cardiol Intv. 2021;14:637-638.
Disclosures
- Shishehbor reports serving as on a global advisory board and consulting with Abbott Vascular, Medtronic, Boston Scientific, Terumo, and Phillips.
- Newby reports external relationships with the ACC, AstraZeneca, Beckman Coulter, GlaxoSmithKline, JACC, National Institutes of Health, Quidel, Roche Diagnostics, and Rockpointe.
- Mukherjee and Lange report no conflicts of interest.





Comments