ISCHEMIA-EXTEND: So Far, Deaths Match for Invasive and Conservative Arms in Stable CAD
Muddying the waters, cardiovascular deaths were reduced in one arm, whereas noncardiovascular were lower in the other.
CHICAGO, IL—(UPDATED) Even with a few more years of follow-up, an initial invasive strategy is no better than a more-conservative approach for improving survival in patients with chronic coronary disease and moderate to severe ischemia, an interim glimpse at ISCHEMIA-EXTEND suggests.
But in a twist that will no doubt continue to complicate the interpretation of these results, cardiovascular deaths were significantly lower among patients randomized to an invasive strategy, whereas noncardiovascular deaths were significantly higher.
Speaking with TCTMD, ISCHEMIA primary investigator David J. Maron, MD (Stanford University School of Medicine, CA), acknowledged that this nuance will perplex physicians and patients alike, but said on the whole that doesn’t matter.
Simply put, “survival is not improved by an invasive approach,” Maron said. “Really the most important thing to a patient is being alive, their overall survival. I don't think the cause of death is as important as whether or not someone is alive or dead. So the major detail that I go over when I'm with patients is overall survival, then if somebody has a particular preference to undergo revascularization to reduce their risk of cardiovascular death, then I try to respect that preference.”
He continued: “It's perplexing that we don't understand the cause of the increase in noncardiovascular death, and so it's going to be difficult to explain that to patients, but the main message really doesn't change.”
As previously reported by TCTMD, the International Study of Comparative Health Effectiveness With Medical And Invasive Approaches (ISCHEMIA) trial found no benefit of an invasive strategy on top of optimal medical therapy (OMT) over OMT alone in preventing a primary endpoint of cardiovascular death, MI, hospitalization for unstable angina, hospitalization for heart failure, or resuscitation due to cardiac arrest over a median 3.3 years in patients with stable, moderate-to-severe coronary artery disease and ischemia based on stress testing. But at that earlier time there were signs that rates of the trial’s original endpoint, cardiovascular death and MI, were lower in the invasive group, warranting a longer look.
Moreover, while interpretations differed depending on how MI was defined and when events occurred, many have speculated that an invasive strategy might ultimately win out, over the longer term.
Commenting on the extended findings, Ajay Kirtane, MD (NewYork-Presbyterian/Columbia University Irving Medical Center, New York, NY), began by reminding TCTMD of the trial’s origins. “When the ISCHEMIA trial was first designed, the idea of the trial was to determine whether a cath-based strategy could ultimately reduce cardiovascular events like cardiovascular mortality and MI. And what I think we're starting to see with these data is that when one looks at those endpoints, certainly MI at the earlier [time point] and now cardiovascular death being reduced by this strategy, that's kind of novel to me and pretty interesting. I think the absolute magnitude of reduction is not huge, but it's not small given how prevalent coronary disease is.”
An Interim Look
Data on all 2,588 patients randomized to an invasive strategy and 2,591 patients randomized to conservative management were included in this interim snapshot, but with varying lengths of follow-up. Sixty-five patients withdrew or declined to participate in the extension study. This particular analysis looked only at all-cause and cardiovascular death, with indeterminate causes being classified as cardiovascular.
It's perplexing that we don't understand the cause of the increase in noncardiovascular death, and so it's going to be difficult to explain that to patients, but the main message really doesn't change. David Maron
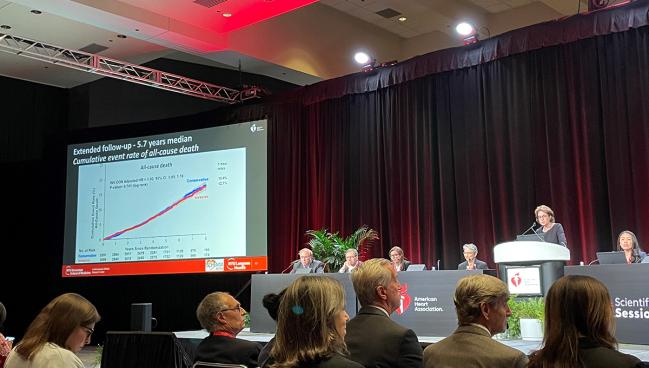
At a median 5.7 years, 557 participants had died, roughly doubling the number of deaths seen in the original trial follow-up. Strikingly, cumulative death rates at 7 years were nearly identical in the two groups: 13.4% in the conservative arm and 12.7% in the invasive arm. (Adjusted HR 1.00; 95% CI 0.85, 1.18).
That’s where the similarities ended. Event curves for cardiovascular deaths began separating 2 years after randomization and by 7 years had reached a rate of 8.6% in the conservative group, as compared with 6.4% in the invasive group. (HR 0.78; 95% CI: 0.63, 0.96).
By contrast, noncardiovascular death rates began to diverge at 3 years, reaching rates of 5.5% in the invasive group and 4.4% in the conservative group at 7 years (HR 1.44; 95% CI 1.08, 1.91). In subgroup analyses there was no interaction found between initial management strategy across a range of prespecified subgroups and all-cause death, CV death, or non-CV death.
In further Bayesian analyses, there was an 82% probability that the invasive strategy is superior to the conservative strategy by at least 1 absolute percentage point for the endpoint of cardiovascular mortality, but an 85% probability that a conservative strategy is superior by at least 1 absolute percentage point for the noncardiovascular mortality endpoint, Maron pointed out to TCTMD.
Thus, as the authors conclude in the published paper: “The probability of near 50% for either a survival benefit with an invasive strategy or a conservative strategy suggests that there is no clinically meaningful difference in 7-year all-cause mortality between groups.”
One group that appears to derive the most marked benefit in terms of reduced cardiovascular deaths from an invasive strategy are patients who have multivessel disease with stenoses of 70% or more, Maron noted. Asked if there was anything he might change about the trial design now, with the benefit of hindsight, to get more definitive answers at this stage of the ISCHEMIA journey, Maron said that limiting the trial population to patients with a 70% narrowing or greater might have given investigators better power to detect a difference.
“In retrospect, if it were possible to recruit enough patients with a minimum 70% narrowing, that would've been to our advantage to find a benefit if one exists,” he said.
Dying of What?
Of note, causes of death are not being centrally adjudicated during the follow-up period, although ISCHEMIA investigators took a deep dive into causes of death in a separate publication earlier this year.
“During the trial phase, we do know that the noncardiovascular deaths were primarily due to cancer and infectious diseases, and we reported in the American Heart Journal the interesting association between radiation exposure and malignancy in the invasive arm: the greater the number of procedures that involve radiation exposure, the greater the risk of a malignancy,” he told TCTMD. “But we know from the radiation and cancer literature that the latency period between exposure to radiation and the development of cancer doesn't fit with our observation,” so this is not currently a working hypothesis.
The same analysis also ruled out the likelihood that a higher use of dual antiplatelet therapy in the invasive arm played any role in increasing malignancy.
Now we see that there is a reduction in cardiovascular mortality just by doing anatomic-based testing, that may make me more apt to think about making the diagnosis. Ajay Kirtane
For Kirtane, who called it “really too bad” that the deaths were not adjudicated beyond the original trial, said the findings are still “useful” for him, as a cardiologist.
“People were, and I myself included, using the ISCHEMIA trial data to sort of say: ‘Listen, you know, at least for the short term—the next three and a half years or so—there's really going to be no difference in events if we just treat you medically.’ But what made me nervous is that if I had a 55-year-old woman in my office to whom I'm saying this; I mean, getting her to 60 is one thing, but what about 65 and 70 and beyond? And that's where longer-term follow-up is important.”
He continued: “Now we see that there is a reduction in cardiovascular mortality just by doing anatomic-based testing, that may make me more apt to think about making the diagnosis, to be more definitive.” That means better defining the anatomy at the outset, said Kirtane, rather than “leaving it at a stress test.” But what ISCHEMIA also made clear is that this doesn’t necessarily mean a trip to the cath lab, Kirtane cautioned. In ISCHEMIA, coronary CT angiography was done to rule out left main disease, and according to Kirtane, that’s one takeaway that many have now implemented in their cath labs.
“I'm totally fine doing a CTA without going to the cath lab and making my decision based upon that,” he said. With these latest data, he said, “you can't tell the patient you're going to save their life overall, but if we can prevent cardiovascular events, then let's at least define the anatomy and then try to figure out what to do based upon that. And I honestly think after ISCHEMIA that's consistent with how people were moving anyway.”
Study chair Judith Hochman, MD (NYU Langone Medical Center, New York, NY), who presented the interim report from ISCHEMIA-EXTEND here at the American Heart Association 2022 Scientific Sessions today, summarized the results to date, saying: “Extended follow-up of the ISCHEMIA randomized trial over a median 5.7 years demonstrated that an initial invasive strategy compared to an initial conservative strategy resulted in no difference in all-cause mortality with nearly twice the number of deaths, a lower risk of cardiovascular mortality, and a higher risk of noncardiovascular mortality. These findings provide evidence for patients with chronic coronary disease and their physicians as they decide whether to add invasive management to guideline-directed medical therapy.”
But the story doesn’t end here, Hochman noted. “Follow-up is ongoing.”
Shelley Wood was the Editor-in-Chief of TCTMD and the Editorial Director at the Cardiovascular Research Foundation (CRF) from October 2015…
Read Full BioSources
Hochman JS, Anthopolos R, Reynolds HR, et al. Survival after invasive or conservative management of stable coronary disease. Circulation. 2022;Epub ahead or print.
Disclosures
- Maron reports having no relevant disclosures.





Comments