Lasers Can Aid Retrieval of Stubborn IVC Filters
Stanford University researchers who pioneered the technique share their latest data on 500 patients treated.
(UPDATED) Laser sheaths can safely and successfully enable retrieval of chronic indwelling inferior vena cava (IVC) filters, according to data on 500 people from a long-running, first-in-human study.
The latest report from William T. Kuo, MD (Stanford University, CA), and colleagues was published earlier this week in the Journal of the American Heart Association.
It’s well established that IVC filters left in place for too long can cause harm. The US Food and Drug Administration advises that the device should come out as soon as possible once acute pulmonary embolism is no longer a risk. But retrieval is often overlooked and sometimes it’s easier said than done, especially when the IVC filters have been in place for several years.
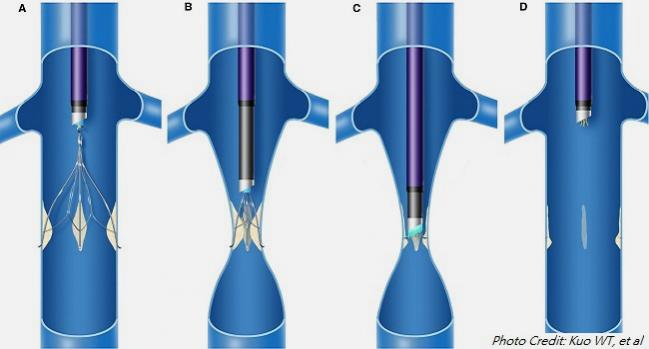
“In these patients, the use of advanced retrieval techniques may be effective, but some centers have reported a risk of major procedure‐related complications when these methods appear to involve excessive force,” the researchers explain. The laser-based approach, not yet FDA-approved, involves fibrotic tissue ablation with less force.
To TCTMD, Kuo explained how they came upon their strategy. “When I began my career at Stanford many years ago, patients with embedded IVC filters came to us because they had no other place to go,” he said in an email. These people were worried about risks posed by their filters but, because their filters had embedded into the caval wall, “standard textbook teaching at the time” was that there was no safe way to remove something that had, in a sense, “converted to permanent.”
We began to wonder if . . . it would be possible to reverse or undo the ‘permanent’ interactions between the vessel and its metallic implant, perhaps on a molecular level. William T. Kuo
He and his colleagues weren’t convinced. “We began to wonder if this was really true and whether it would be possible to reverse or undo the ‘permanent’ interactions between the vessel and its metallic implant, perhaps on a molecular level,” Kuo said. Eventually, their efforts led them to the discovery of excimer laser-assisted retrieval and they launched a dedicated clinic to serve these hard-to-treat cases.
Over an 8.5-year period at Stanford’s IVC Filter Clinic, 2,500 patients underwent attempted retrieval using advanced methods beyond standard snaring/sheathing. Even with these techniques, retrieval wasn’t successful for 500 when using three times the standard force (6 to 7 pounds). And so treatment was escalated via a laser sheath connected to a 308‐nm XeCl excimer laser generator (CVX-300; Spectranetics).
Among these 500 patients, mean age was 49 years and 55% were women. Most of the devices had been designed to be retrievable, with 17.2% being permanent. Mean IVC filter dwell time was 1,528 days. Reasons for retrieval included:
- Filter-related morbidity (symptomatic acute inferior vena cava thrombosis, chronic inferior vena cava occlusion, and/or pain from filter penetration), in 28%
- Anxiety—but without symptoms—over the potential risks posed by an indwelling filter and the desire to prevent complications, in 72%
- With or without symptoms, the goal of quitting long-term anticoagulation that had been necessitated by the IVC filter, in 16%
Laser-assisted retrieval was successful in 99.4% of the 500 cases, with an average force of 3.6 pounds. Major complications were seen in 10 patients (2%), none occurring in the last 1.5 years of the study period. All were successfully treated with medical management and/or percutaneous endovascular therapy.
Retrieval enabled all but one of the 78 patients originally on anticoagulation to stop taking their medication within a few months of the procedure. For the 140 patients who had filter-related morbidity prior to IVC filter removal, it resolved the symptoms in 98.5%. “Among patients with no physical filter-related morbidity, none developed any major procedure-related complications, and all reported relief of filter-related anxiety and achieved cessation of filter-related anticoagulation (if previously prescribed) following filter removal,” the researchers report.
Expertise Is Key
Kuo et al stress that these advanced methods must be done at experienced centers. Tracking their own complications, as part of this study, enabled them to more safely perform these procedures over time, they point out. “Essentially, we learned from this larger experience that venous vascular injury and thrombosis are just a few of the complications that may occur as previously described and that retrieval of penetrating filter components may also be associated with major arterial hemorrhage, organ injury, and sepsis.”
Kush R. Desai, MD (Northwestern University, Chicago, IL), whose group is also researching laser-assisted removal, described Kuo as a “pioneer in this area.”
Over time, advanced retrieval techniques as a whole have “become much more generalized,” Desai said, adding, “What started as a very niche practice has really proliferated, and there’s a bunch of people taking out filters and many of them are using the laser.”
Based on his own findings, recently published in JAHA, “there are certain filter designs [where] frankly without the laser I don’t think we would’ve gotten them out or certainly not have gotten them out as safely,” Desai noted. “But I don’t think that applies to all filters.” Specifically, Desai et al found closed-cell filters were much more likely to require laser than were open-cell filters (60% vs 7%; OR 20.1; 95% CI 11.5-36.7).
Each group has its own take on how best to handle these complex cases, he emphasized. As mentioned in the paper by Kuo et al, another option is the use of endobronchial forceps. Desai said that, for him, the laser offers “a little bit more control of the procedure. I don’t have to pull quite as hard . . . with the laser as I do with the forceps.”
Desai, too, drew attention to the fact that complication rates of laser-assisted retrieval are low, with this level of safety thanks to the cases being done at expert centers.
He urged a broad perspective on IVC filters, commenting: “It’s much more of a global thing than just retrieval. It’s about: which patients should get a filter? How should we monitor those patients? How do we improve retrieval rates so that we’re not talking about using lasers and [other techniques so] that the number of complex retrievals we’re doing goes down? Ultimately, I think patients are better served that way.”
To TCTMD, Kuo said that once the decision has been made to remove an IVC filter, several factors should be weighed when considering the need for laser assistance. These include “device type, device complications, vessel condition, length of dwell time, and prelaser force-gauge reading to assess amount of scar tissue (and whether laser is even needed),” he noted, adding that what’s most crucial are the “operator’s experience and comfort level with advanced retrieval techniques.”
He described a former patient who had undergone laser-assisted filter removal at another center: “The case was complicated by the filter embolizing from the IVC into the heart, and that patient was emergently airlifted to Stanford Hospital for further care. Fortunately, we were able to remove that filter percutaneously and avoid the need for open CT surgery. My point is that laser availability does not ensure success, and lack of appropriate expertise/training may lead to potentially fatal complications.”
Prospective study of laser-assisted retrieval continues at Stanford, Kuo said. “We aim to continue gathering data for further validation in even larger cohorts. We also need to study how the nuances of this technique apply specifically to each of the many filter types encountered and to a growing variety of complex cases and scenarios referred to us.”
Photo Credit: “Illustration of laser‐assisted filter retrieval,” by Kuo WT et al, is licensed under CC BY 2.0
Caitlin E. Cox is Executive Editor of TCTMD and Associate Director, Editorial Content at the Cardiovascular Research Foundation. She produces the…
Read Full BioSources
Kuo WT, Doshi AA, Ponting JM, et al. Laser‐assisted removal of embedded vena cava filters: a first‐in‐human escalation trial in 500 patients refractory to high‐force retrieval. J Am Heart Assoc. 2020;Epub ahead of print.
Disclosures
- Kuo reports no relevant conflicts of interest.
- Desai reports being a consultant and on the speaker’s bureau for Cook Medical, Boston Scientific, Philips/Spectranetics, W.L. Gore, Becton Dickinson/Bard, and Walk Vascular.


Comments